Medial Epicondyle Tendinopathy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 96: | Line 96: | ||
== Key Research == | == Key Research == | ||
Hoogvliet, P. ,Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review, (Ann Rehabil Med. 2012 Oct).., geraadpleegd op 2 mei 2014, http://www.ncbi.nlm.nih.gov/pubmed/23709519 level of evidence 1A<br> | |||
== Resources <br> == | == Resources <br> == | ||
Revision as of 13:01, 14 July 2014
Original Editors - Anouk Toye
Top Contributors - Sanne Delporte, Anouk Toye, Darrell Blommaert, Shaimaa Eldib, Admin, Alynn De Maeyer, Rachael Lowe, Lauren Lopez, Fasuba Ayobami, Kim Jackson, Kai A. Sigel, 127.0.0.1 and Naomi O'Reilly
Search Strategy[edit | edit source]
I would recommend to consult PubMed. The keywords I used to become several references were:
- ‘medial epicondylitis’ (108 results – 12 free full texts)
- ‘medial epicondylitis AND physical therapy’ (11 results – 1 free full text)
- ’medial epicondylitis AND diagnosis’ (81 results - 7 free full texts)
- ’medial epicondylitis AND treatment’ (75 results – 7 free full texts),
- ‘Golfer’s elbow’ (19 results – 2 free full text)
- ‘Golfer’s elbow test AND physical therapy’ (3 results)
- ‘Golfer’s elbow AND diagnosis’ (12 results – 2 free full texts)
- ‘Golfer’s elbow AND treatment’ (15 results – 1 free full text).
It’s also very helpful to check the references of each usable article.
Other sites to consult are Web of knowledge, Sholar.google.com and Books.google.com.
Definition/Description[edit | edit source]
Medial epicondylitis is mostly an overload injury. The most sensitive region is located near the origin of the wrist flexors on the medial epicondyle of the humerus. Sometimes the patient also experiences pain on the ulnar side of the forearm, the wrist and occasionally in the fingers. Although epicondylitis means there is an inflammation, there is some controversy with this pathology. Histologically it has been shown that medial epicondylitis is the result of microtearing in the tendon that isn’t fully relapsed (=To fall or slide back into a former state). Some physical therapists prefer the term tendonosis instead of epicondylitis.[1]
In some cases, the symptoms of golfer's elbow (medial epicondylitis) are due to inflammation. In an acute injury, the body undergoes an inflammatory response. Special inflammatory cells make their way to the injured tissues to help them heal. Conditions that involve inflammation are indicated by -itis on the end of the word. For example, inflammation in a tendon is called tendonitis. Inflammation around the medial epicondyle is called medial epicondylitis.
However, golfer's elbow often is not caused by inflammation. Rather, it is a problem within the cells of the tendon. Doctors call this condition tendonosis. In tendonosis, wear and tear is thought to lead to tissue degeneration. A degenerated tendon usually has an abnormal arrangement of collagen fibers.
Instead of inflammatory cells, the body produces a type of cells called fibroblasts. When this happens, the collagen loses its strength. It becomes fragile and can break or be easily injured. Each time the collagen breaks down, the body responds by forming scar tissue in the tendon. Eventually, the tendon becomes thickened from extra scar tissue. [2]
These conditions are most of the time caused by a constant trauma and tension of the tendon attachment to the medial epicondyles. In some cases it can also emerge spontaneously.
Clinically Relevant Anatomy[edit | edit source]
Osteology: Medial epicondyle of the Humerus
Musculature: Wrist Flexor Group
- M. pronator teres
- M. flexor carpi radialis
- M. palmaris longus
- M. flexor digitorum superficialis
- M. flexor carpi ulnaris
All these muscles have the same origin: the medial epicondyle.[3]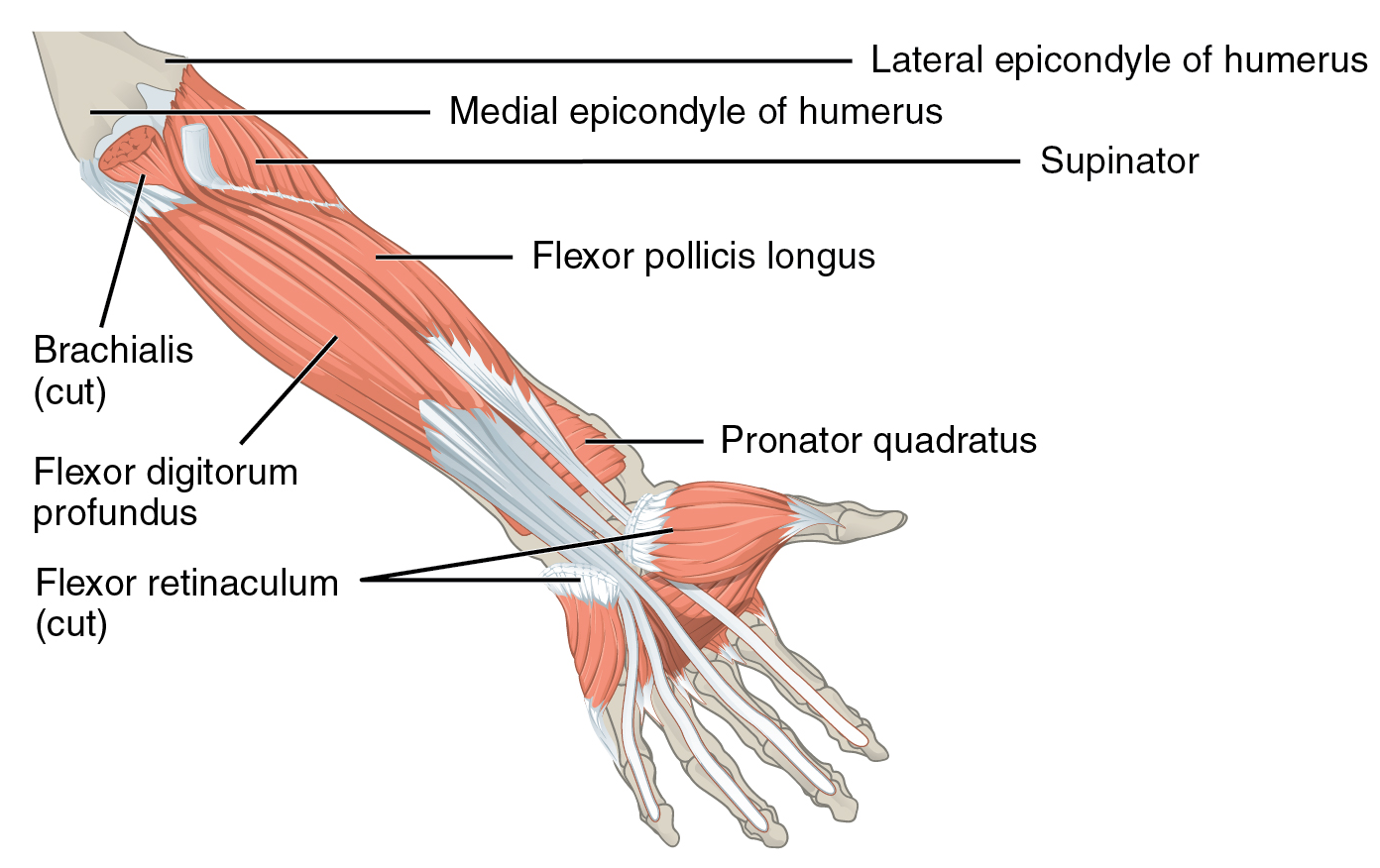 [4]
[4]
Epidemiology /Etiology[edit | edit source]
Its pseudonym ‘golfer’s elbow’ is easily remembered but misleading as 90 to 95% of all cases do not involve sportsmen (level of quality A2)[5] (level of quality D)[6]. Symptoms may be produced by sudden violence to these tendons by repeated usage or by chronic strain. In many cases trauma at work had been identified as the cause of the symptoms (level of quality A2)[5].
More specific occupational physical factors associated with medial epicondylitis are forcefull activities among men and with repetitive movements of the arm among women.
Current smoker and former smoker are also associated with medial epicondylitis, so do patients who suffer from diabetes type 2 (level of quality A2)[5].
Characteristics/Clinical Presentation[edit | edit source]
As medial epicondylitis is an inflammation of the tendon of the flexor group attached to the medial epicondyle of the humerus, the most sensitive region will be located near the origin of the wrist flexor group.
The patient usually complains of pain about the elbow distal to the medial epicondyle of the humerus with radiation up and down the arm, most common on the ulnar side of the forearm, the wrist and occasionally in the fingers (level of quality A1)[7].
Other characteristics are the local tenderness over the medial epicondyles and the conjoined tendon of the flexor group, without evidence of swelling or erythema.
The pain evokes by resisted flexion of the wrist end by pronation. The pain usually notices a weakness of hand grip (level of quality A1)[7].
Pain can begin suddenly or can develop gradually over time.
You might have a harder time with activities that require arm strength, including sports that require you to hit backhand or throw a ball. (level of evidence A1)[8]
Differential Diagnosis[edit | edit source]
When diagnosing a medial epicondylitis, the therapist always has to consider other pathologies such as[1][9]:
- a compression neuropathy of the ulnar and the median nerve
- ulnar collateral ligament instability
- ulnar neuritis (Cubital Tunnel Syndrome II) --> Ulnar Nerve Entrapment
- Obsessive compulsive disorder (OCD)
- Medial collateral ligament sprain --> Elbow Ligamentous Injuries
- Adhesive_Capsulitis
- Cervical_Radiculopathy
- Osteoarthritis
- Flexor-pronator strain
The use of Polk's_Test may help the clinician to diagnostically differentiate between lateral en medial epicondylitis. Other various orthopedic testing procedures including Cozen’s_Test, Golfer’s_Elbow_Test, Mill’s_Test and Kaplan’s test are used for the clinical differentiation between lateral en medial epicondylitis (level of quality D) [6].
Diagnostic Procedures[edit | edit source]
As epicondylitis is essentially a musculotendinous condition, diagnosis is essentially clinical.
Radiographs are typically negative unless the chronicity of the condition had allowed periostitis to develop on the affected epicondyle (level of quality D)[6].
The diagnosis of medial epicondylitis is based on local pain at the elbow, tenderness at the epicondyle on palpation and pain at the epicondyle on resisted isometric flexion and pronation of the wrist (level of quality A1)[10] (level of quality A2)[5].
In particular the Golfer’s_Elbow_Test, an orthopedic test, is described as being helpful to diagnose medial epicondylitis (level of quality D)[6].
Outcome Measures[edit | edit source]
Medial epicondylitis test( level of evidence 1) [11]
A passive and active test to determine medial epicondylitis. In severe cases of epicondylitis, the person will complain of pain if he simply shakes hands or pulls an open door.
For the active resistance test, resist wrist flexion . This must be carried out with elbow extended while fully supinating the forearm.
For the passive test, extend the wrist with the elbow extended.
Examination[edit | edit source]
- Tenderness to palpation (usually over m. pronator teres and m. flexor carpi radialis)
- Local swelling and warmth
- Range of motion in the beginning of the disease can be full, but later on there is a possibility of a decreased range of motion[12]
Medical Management
[edit | edit source]
Surgical treatment of medial epicondylitis
When conservative management fails and there is persistent pain after 6 to 12 months and all other pathologies are considered, surgical treatment must be considered.
Surgery for failure of conservative treatment relieves pain, restored strength and allows a return to the previous level of daily living and sports activity (level of quality C)[13].
Mini-open muscle resection procedure under local anesthesia
For medial epicondylitis the degenerative tissue at the origine of the flexor carpi radialis brevis is removed during a mini-open muscle resection procedure.
This procedure produces low levels of postoperative pain, a short hospital stay and rehabilitation period and early return to daily activities.
The limitations of and open flexor carpi radialis brevis release include late return to work and sporting activities due to a prolongation of the postoperative recovery time, a risk of posterolateral instability, and the formation of nueroma after surgery (level of quality B)[14].
Fascial elevation and tendon origin resection (FETOR)
Fascial elevation and tendon origin resection facilitates the complete visualization and resection of the CFPO (Chronic Flexor Palmar Origin) with limited soft tissue dissection.
FETOR decreases the average pain, pain at rest, and pain during hard work or heavy lifting. There is also an improvement of the mean pain-free grip strength. (level of evidence 4)[15]
Steroïd injections
The indication for injection therapy for epicondylitis is usually chronic pain and disability not relieved by more conservative means, or severe acute pain with functional impairment that calls for a more rapid intervention.
These injections seem to have a short term effect ( 2-6 weeks) and effective in providing early symptom relief (level of quality A1)[10].
Initial extracorporeal shock wave therapy is effective for the patients newly diagnosed as medial epicondylitis although the effectiveness on completion of the treatments were inferior than local steroid injection. Therefore, extracorporeal shock wave therapy can be another option when local steroid injection is contraindicated. (level of evidence 1B) [16]
Autologous blood injection
The combined treatment of dry needling and ultrasound guided autologous blood injection is discribed as a effective way to treat patients with refractory lateral and medial epicondylitis. The hypothesis of the mechanism is that the transforming growth factor-β and basic fibroblast growth factor carried in the blood act as humoral mediators to induce the healing cascade (level of quality C)[17].
Physical Therapy Management
[edit | edit source]
Nonsurgical treatment
The main goal of the conservative treatment is to obtain pain relieve and an inflammation reduce. These two things will help to achieve a proper rehabilitation and later a return to activities.
Nonsurgical treatment can be divided into three phases.
- Phase 1: The patient immediately has to stop the offending activities. It’s not recommended to stop all activities or sports since that can cause atrophy of the muscles.
The therapy starts with ‘PRICEMM’, which stands for ‘prevention/protection, rest, ice, compression, elevation, modalities and medication'. The affected elbow should be iced several times a day for about a quarter. This improves the local vasoconstrictive and analgesic effects. As for medication the patient can take nonsteroidal anti-inflammatory medication (NSAID).
If the patient’s condition doesn’t improve, a period of night splinting is adequate. This is usually accompanied with a local corticosteroid injection around the origin of the wrist flexor group. Some examples of a physical therapy modality are ultrasound and high-voltage galvanic stimulation (but there’s not yet a study that notes their efficacy).
Counterforce bracing is recommended for athletes with symptoms of medial epicondylitis. It can also aid when the patient is returning to sport.
- Phase 2: As soon as we see an improvement of phase 1, a well guided rehabilitation can be started. The first goal of the second phase is to establish full, painless, wrist and elbow range of motion. This is soon followed by stretching and progressive isometric exercises. These exercises first should be done with a flexed elbow to minimize the pain. Although not yet conclusive, is the belief that strength training decreases symptoms in tendinosis. The short-term analgesic effect of manipulation techniques may allow more vigorous stretching and strengthening exercises resulting in a better and faster recovery process of the affected tendon in Medial epicondylitis. (A1) [18]As soon as the patient has made some progress the flexion of the elbow can be decreased. As the flexibility and the strength of the elbow area return, concentric and eccentric resistive exercises are added to the rehabilitation program. The final part of this phase is a simulation of sport or occupation of the patient.
- Phase 3: When the patient is able to return to his sport it is necessary to take a look at his equipment and/or technique. These precautions ought to be taken to allow a safe return to activities (level of quality D)[12].
Postoperative management
7 to 10 days after the operation, the splint and skin sutures are removed. At this point the physical therapy can start. The beginning of the treatment is characterized by gentle passive and active hand, wrist and elbow exercises. 3 to 4 weeks later gentle isometrics can be done and at 6 weeks the patient can start with more resistive exercises. At last a progressive strengthening program has to be followed. In normal cases the patient can return to activities 3 to 6 months after the operation (level of quality D)[12].
Prevention [edit | edit source]
A healthy elbow requires a healthy shoulder and wrist joint and strong muscles around the scapula (shoulder blades) and arms to decrease the load on the smaller forearm muscles.
To prevent overuse and strain in the elbow and forearm:
-Take frequent breaks from activities that require extensive hand/wrist motions.
-Reduce or avoid lifting objects with the arm extended.
-Reduce repetitive gripping and grasping with the hand and wrist. Decrease the overall tension of gripping.
-Avoid the extremes of bending and full extension.
-Work or weight-train with the elbow in a partially bent position. Use wrist supports when weight-training.
-When using tools, increase the gripping surface by wearing gloves or adding padding. Use a hammer with extra padding to reduce tension and impact. Hold heavy tools with two hands.
-Use a two-handed backhand in tennis. When hitting a tennis stroke, use your entire lower body, hip, pelvis, and back, and use less of your elbow. Using the proper technique in tennis can help reduce symptoms. Reevaluate the size of your grip, string tension, type of string, new strokes, and new grips for new strokes, which can all contribute to problems.
-Some suggest lowering string tension, finding the heaviest racket that does not affect your swing speed, finding the largest grip that is comfortable, and using softer strings.
-Apply grip tape or an oversized grip on golf clubs. (level of evidence A1)[19]
Key Research[edit | edit source]
Hoogvliet, P. ,Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review, (Ann Rehabil Med. 2012 Oct).., geraadpleegd op 2 mei 2014, http://www.ncbi.nlm.nih.gov/pubmed/23709519 level of evidence 1A
Resources
[edit | edit source]
Clinical Bottom Line[edit | edit source]
add text here
References[edit | edit source]
- ↑ 1.0 1.1 Richard B. Birrer, Francis G. O’Conner, Sports medicine for the primary care physician, 3th Edition, 2004, CRC Press LLC, Boca Raton, Florida fckLRQuality: secondary resource
- ↑ http://www.methodistorthopedics.com/medial-epicondylitis-golfers-elbow
- ↑ R. Putz , R. Pabs, Sobotta atlas of human anatomy, 3th Edition, 2006, Bohn Stafleu van Loghum, Houten, p180fckLRQuality: Secondary resource
- ↑ The Mcgraw-Hill Companies, geraadpleegd op 4 mei, http://www.rci.rutgers.edu/~uzwiak/AnatPhys/APFallLect15_files/image023.jpg
- ↑ 5.0 5.1 5.2 5.3 SHIRI R. et al, Prevalence and determinants of the lateral and medial epicondylitis: a population study, American journal of epidemiology, September 2006, vol. 164 n° 11, pag 1065 – 1074, level of quality A2
- ↑ 6.0 6.1 6.2 6.3 POLKINGHORN B.S., A novel method for assessing elbow pain resulting from epicondylitis, Journal of chiropractic medicine, 2002, vol. 1 n° 3, pag. 117 – 121, level of quality D
- ↑ 7.0 7.1 MARMOR L, Medial epicondylitis, July 1959, vol. 91 n° 1, pag.23, level of quality A1
- ↑ Jayanthi, N. (2013). http://www.uptodate.com/contents/elbow-tendinopathy-tennis-and-golf-elbow-beyond-the-basics?view=print, geraadpleegd op 2 mei 2014. Level of evidence 1A
- ↑ Walter R. Frontera, Julie K. Silver, Thomas D. Rizzo, Jr. Essentials of physical medicine and rehabilitation; musculoskeletal disorders, pain, and rehabilitation, 2nd edition, 2008, by Saunders , an imprint of Elsevier Inc.fckLRQuality: Secondary resource
- ↑ 10.0 10.1 CARDONE D.A., TALLIA A.F., Diagnostic and therapeutic injection of the elbow region, American family physician, December 2002, vol. 66 n° 11, pag. 2097 – 2100, level of quality A1
- ↑ Sandra J. Shultz, Peggy A. Houglum, David H. Perrin. Examination of musculoskeletal injuries. USA, Human Kinetics, 2000, p295.level of evidence 1A
- ↑ 12.0 12.1 12.2 Michael C. Ciccotti , MA, RA, Michael A. Schwartz, MD, Michael G. Ciccotti, MD. Diagnosis and treatment of medial epicondylitis of the elbow. Clin Sports Med 23 (2004) 693-705fckLRQuality: D4
- ↑ VANGSNESS C.T., JOBE F.W., Surgical treatment of medial epicondylitis, The journal of bone and joint surgery, May 1991, vol. 73B n° 3, pag. 409 – 411, level of quality C
- ↑ CHO B.K. et al, Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis, Clinics in orthopedic surgery, 2009, vol. 1 n° 3, pag. 123 – 127, level of quality B
- ↑ Kwon, BC. (2014).The Fascial Elevation and Tendon Origin Resection Technique for the Treatment of Chronic Recalcitrant Medial Epicondylitis., geraadpleegd op 2 mei 2014, http://www.ncbi.nlm.nih.gov/pubmed/24758782 level of evidence 4
- ↑ Lee SS. Et al, Effectiveness of initial extracorporeal shock wave therapy on the newly diagnosed lateral or medial epicondylitis, Ann Rehabil Med, 2012 Oct., geraadpleegd op 2 mei 2014, http://www.ncbi.nlm.nih.gov/pubmed/23185733 level of evidence 1B
- ↑ SURESH S.P.S., ALI K.E., JONES H., CONNELL D.A., Medial epicondylitis: is ultrasound guided autologous blood injection an effective treatment?, biomedical journal of sports medicine, September 2006, pag. 935 – 939, level of quality C
- ↑ Hoogvliet, P. (2013). Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review., (Ann Rehabil Med. 2012 Oct).., geraadpleegd op 2 mei 2014, http://www.ncbi.nlm.nih.gov/pubmed/23709519 level of evidence 1A
- ↑ Jayanthi, N. (2013). http://www.uptodate.com/contents/elbow-tendinopathy-tennis-and-golf-elbow-beyond-the-basics?view=print, geraadpleegd op 2 mei 2014. Level of evidence 1A
add references here - see adding references tutorial for help






