Multiligament Injured Knee Dislocation
***Editing in process***
Original Editors - Caro De Koninck
Top Contributors - Estelle Hovaere, Leana Louw, Caro De Koninck, Admin, Kim Jackson, 127.0.0.1, Evan Thomas, Daphne Jackson, WikiSysop, Naomi O'Reilly and Wanda van Niekerk
Definition/Description[edit | edit source]
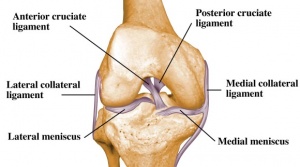
A multi-ligament-injured knee is commonly misnamed knee dislocation in medical literature. A dislocation causes a complete joint disruption, resulting in the loss of contact of the articular surfaces. Subluxation occurs when the articular surfaces stay in contact.[1] Both of these fall under the term "multi-ligament-injured knee". A multi-ligament-injured knee is caused by injury of at least two out of the 4 major knee ligaments (namely ACL, PCL, LCL and MCL), normally associated with considerable ligamentous disruption.[1][2][3] It causes disruption of the active and passive stabilizers of the knee joint and is often linked with compromise to neurovascular structures and can potentially be limb theatening.[4]
Clinically relevant anatomy[edit | edit source]
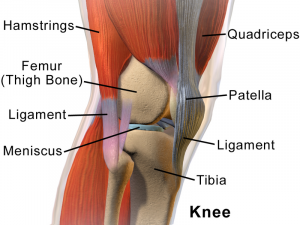
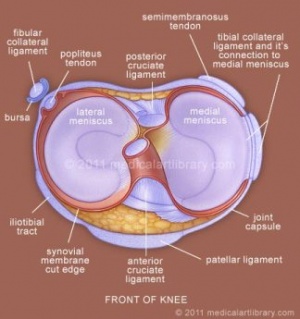
The knee joint is made up of articulations of the distal femur, proximal tibia and patella.[4]
Ligaments:[4]
\
Menisci:[4]
Muscles:[4]
- Anterior:
- Quadriceps
- Lateral:
- Iliotibial band
- Biceps femoris
- Popliteus
- Medial:
- Pes anserinus (sartorius, gracilis, semitendinosus)
- Semimembranosus
- Posterior:
Vasculature:[4]
- Femoral artery
- Popliteal artery
Innervation:[4]
- Terminal branches of the following nerves:
- Cutaneous nerves:
- Posterior & lateral femoral cutaneous
- Lateral sural cutaneous
- Saphenous
- Obturator
Medial stabilizers of the knee (against valgus stress):[4]
- Superficial: Sartorius, fascia
- Middle: Posterior oblique ligament, semimembranosus, MCL
- Deep: Joint capsule, medial capsular ligament
Posteriolateral stabilizers of the knee:[4]
- Superficial: Iliotibial band, biceps femoris, fascia
- Middle: Patellar retinaculum, patellofemoral ligaments
- Deep: LCL, popliteus tendon, popliteofibular ligament, fabellofibular ligament, arcuate ligament, joint capsule
See the page on the knee joint for in-depth information the anatomy and kinematics of the knee. This background is needed to understand knee dislocations better.
Epidemiology /Etiology[edit | edit source]
Knee dislocation is estimated to be less than 0,2% of all orthopedic injuries. Total knee dislocations are rare and usually happen after major trauma, including falls, car crashes, and other high-speed injuries.[3] Spontaneous dislocation is often seen in cases associated with obesity.[2] Knee dislocations can also present in congenitally and has an incidence of approximately 1 per 100,000 live births. 40-100% of these cases have additional musculoskeletal anomalies.[5]
- Anterior dislocation = 40%
- Posterior dislocation = 33%
- Medial dislocation = 4%
- Lateral dislocation = 18%
- Rotary dislocation = 5%
- Complete disruption of all 4 major knee stabilizing ligaments: 11%
Low-velocity injuries - morbid obese (trivial trauma), lax ligaments
High velocity knee injuries 30% vascular injury - high
41% popliteal artery injury
41% neurologic injury with 50% chance of neurologic recovery at follow-up; 71% peroneal, 29% peroneal and tibial; 29%AKA
Complications[edit | edit source]
- Vascular disruption
- Common peroneal nerve injuries
- Iatrogenic vascular injury
- Arthrofibrosis
Characteristics/Clinical presentation[edit | edit source]
Most multi-ligament knee injuries are easily reducible with minimal assistance or even spontaneous.[1] Dislocation can be suspected based on physical exam findings of joint instability/ligamentous injuries, but also based on hemarthosis and tenderness to palpation.[6] It is often difficult to diagnose if a reduced knee was dislocated or subluxed without clinical witness or radiological evidence.[1] Associated meniscal, osteochondral, and neurovascular injuries are often present and can complicate management.[7]
Knee dislocations occur in 5 main types: Anterior, posterior, medial, lateral and rotary. Anterior dislocations represent more than 70% of knee dislocations. Rotary dislocations can further be divided into anteromedial, anterolateral, posteromedial and posterolateral injuries.[8]
Mechanism of injury:[3]
- Anterior dislocation: Hyperextention force
- Posterior dislocation: Anterioposterior force (e.g. dashboard injury)
- Medial dislocation: Varus force (often associated with tibial plateau fractures)
- Lateral dislocation: Valgus force (often associated with tibial plateau fractures)
- Rotary dislocation: Combination of forces
Classification:[3]
- Acute: < 3 weeks post injury
- Chronic: > 3 weeks post injury
Associated injuries:[3]
- Popliteal artery (19%)
- Common peroneal nerve (20%)
- Vascular injuries (19%):
- High-velocity injury (65%)
- Low-velocity injury (4.8%)
- Fractures (including avulsion) - distal femur, proximal tibia (16%)
- Compartment syndrome
Ligamentous injuries have characteristics such as:
- Long-term joint instability
- Patient’s mobility
- Quality of life
The most common problems of knee dislocation are stiffness, secondary to arthrofibrosis or failure of a ligament repair or reconstruction. In the long term, it is reported that up to 50% of patients may develop post-traumatic Osteoarthritis
Compartment syndome - ischaemic & compression nerve injury
Differential Diagnosis[edit | edit source]
Classifications of knee dislocations have been based on either an anatomical and/or a positional scheme. The positional classification categorizes knee dislocations according to the tibial position in relation to the femur also known as the Kennedy Classification, named after the author in 1963. Five types were initially defined [2] :
- anterior (Fig. 1)
- posterior (Fig. 2)
- lateral
- medial
- rotatory
Rotatory knee dislocations were subdivided into four groups: anteromedial, anterolateral, posteromedial and posterolateral.
Although well established and useful, the positional classification system has limitations. Up to 50% of knee dislocations are spontaneously reduced before evaluation and cannot be classified with the positional classification. Therefore an anatomical system was developed, based on ligament injury with additional designations of C (arterial injury) and N (neural injury)[9].
KDI is described as —> a single cruciate tear
KDII —> bicruciate tears without collateral tears
KDIIIM —> bicruciate tears with involvement of a medial collateral ligament
(MCL) KDIIIL —> involvement of a lateral collateral ligament (LCL) and
posterolateral corner (PLC) tear
KDIV —> involves all four ligaments and KDV involves a fracture-dislocation.
In general, the higher the number, the greater the injury to the knee.
Diagnostic procedures[edit | edit source]
It is easy to diagnose the unreduced knee, but as most cases present already reduced, it is important to do a thorough evaluation to make an accurate diagnosis and to exclude any potential associated injuries.[3] Patients normally come in with a complaint of severe pain and instability, limiting activities of daily living and sport. Physical examination of a patient with a suspected knee dislocation should take place shortly after the injury is sustained.[10] Knee dislocation often goes hand-in-hand with concomitant injuries to other structures such as nerves and blood vessels. It is very important to do a neurovascular assessment to exclude injuries to perineal nerve and popliteal artery.[11] X-rays are recommended to exclude any fractures.
All cases of suspected knee dislocation should have an ankle-brachial index performed, reserving arteriography for those with an abnormal finding. (Levy et al., 2010, A1)[10]
Examination[3][edit | edit source]
It is very important to do thorough and repeated evaluation of the neurological and vascular status for signs of injury to the common peroneal nerve, popliteal artery and to assess for compartment syndrome.
Ankle-brachial index: Can be used to determine if angiography is needed (threshold of <0.9 can positively predict a vascular injury in need of surgery)
Observation:
- Unreduced knee
- Swelling and bruising - uncontained haemarthrosis is a major finding that can lead to the diagnosis of knee dislocation; it also suggests disruption of the joint capsule
Palpation: Diffuse pain present
Range of motion: Decreased
Ligament testing: This might be challenging to do in the acute, reduced knee as a result of pain and discomfort [8]
- PCL and posterior capsule disruption - hyperextention on passive elevation of knee
- Varus and valgus laxity tested in full extention - indication of associated capsular disruption
- Lachman's test: Laxity present in anterior and posterior directions as a result of disruption of the cruciate ligaments
- Anterior drawer: Not recmmended, as it is challenging to perform and reliability is compromised as a result of pain, loss of range of motion and muscle spasms
- Pivot-shift and reverse pivot-shift test: Not recommended in acute cases, extremely difficult to test with swollen knee where MCL is disrupted; works well in chronic cases
- Dail test: PCL and posterolateral corner involvement when finding of increased external rotation of the tibia is present
- Examination of pulses: This is necessary to make sure there are no any
injuries to the arteries. The physician will search for a pulse in the foot. - An arteriogram (X-ray of the artery): This X-ray is necessary to detect
injuries to the artery. Some medical centers may also use special
ultrasound or Doppler machines to assess the blood flow in the arteries.
Although there is proof that physical examination of the popliteal artery is
accurate enough to rely on. The presence or absence of an injury of the
popliteal artery after knee dislocation can be safely and reliably predicted,
with a 94.3% positive predictive value and 100% negative predictive
value.[2] - Examination of nerves: It is possible that the nerves may have been
damaged. Moving the foot up and down and turning the foot inside
(inversion) and outside (eversion) are important muscle movements to
examine. Any feeling of numbness is an indicating sign for nerve damage.[6]
Outcome Measures[edit | edit source]
Recent prospective studies declare that patients who achieve a good Lysholm score, could perform activities on a regular basis and could perform hop tests comparable to the other knee.[2]
Medical Management[edit | edit source]
Knee dislocations should be reduced as soon as possible. An angiogram should be done to investigate if any vascular injuries are present.[11]
Knee dislocation with vascular injury:[11]
- Vascular repair
- Repair posterior capsule tear
- Knee stabilization with a range of motion brace (e.g. Donjoy/Exoskeleton)
- Remaining instability should be addressed at a later stage
Knee dislocation without a vascular injury:[11]
- Primary repair (when swelling permits)
- Stabilize in a plaster of paris cast or range of motion brace (e.g. Donjoy/Exoskeleton)
Definitive management of acute knee dislocation remains a matter of debate. Surgical reconstruction of the collateral ligaments, the cruciate ligaments, and the PCL on the contrary seems way better.Also Henrichs (2004, A1)[2] says that surgical treatment had proven to be much more beneficial for active patients. Conservative treatment on the other hand is often chosen if the joint feels relatively stable postreduction or if the patient is older or sedentary with intact colletarel ligaments.Conservative treatment means applying a brace that limits the range of motion of the knee.[12]
Patients who are diagnosed with knee dislocation at birth are examined within 24 hours after birth. Treatment with conservative methods at an early stage is most likely to yield successful results. These conservative methods include direct reduction under gentle, persistent manual traction.[13]
There are also non-conservative methods that can be used later on such as Percutaneous quadriceps recession (PQR) and V–Y quadricepsplasty. [2]After both procedures an above knee cast is applied to ensure knee flexion. Important is that the cast does not push the tibial plateau to anterior and therefore re-dislocate the knee. After six weeks the cast is removed. No splints or physiotherapy are advised.[2]
Percutaneous quadriceps recession (PQR) as described by Roy & Crawford (1989): Medial and lateral stab incisions are made at the superior border of the patella to divide the medial and lateral quadriceps and retinaculum. The knee is then forced into flexion, while applying direct forward pressure on the femoral condyles with the fingers.[8]
V–Y quadricepsplasty as described by Curtis and Fisher (1969): There is made an incision in the central part of the quadriceps tendon in a fashion that allows V–Y advancement. The iliotibial band is released. The anterior capsule of the knee is divided transversely as far as the collateral ligaments, and the quadriceps muscle is mobilized. The knee is then reduced and flexed to 90°. The lengthened quadriceps is resutured with the knee held at 30°. This treatment has a higher morbidity compared with the PQR due to a long incision with scarring, adhesions,and wound breakdown, as well as blood loss. However, V-Y quadricepsplasty is more successful in attaining and prolonging reduction in severe and resistant cases.[8]
Physical Therapy Management
[edit | edit source]
Treatment is dependent of the damaged structures. Each patient will have a different treatment which depends on the current stability of the patient, and eventually the other injuries that occurred in the injured limb. The ultimate goal of the therapy is to restore stability and regain a pain free functional mobility.[5]
Depending on the medical treatment given, there are 2 rehabilitation programs:
- Nonoperative treatment:
Allows the healing of the capsular and collateral ligaments so that varus and valgus stability can be restored
- 6 to 8 weeks initial mobilization
- Weight bearing exercises
- Passive and active training of the range of motion
- Muscle strengthening
After conservative treatment, rehabilitation may begin immediately. The first exercises are upper and midbody exercises, along with single-leg stationary bicycling in order to maintain
cardiovascular conditioning. Quadriceps strengthening is important to prevent patellofemoral problems during rehabilitation. During early exercises, wearing a brace is important to limit ROM from 90°of flexion to 45°of extension. Light manual-resistance exercises may be performed in this range as tolerated. As the patient progresses, other resistance machines such as Biodex may be used in place of manual therapy. After 8 weeks of rehabilitation, the patient may begin doing exercises with a leg-press machine. During this face, the knee needs only minimal protection. These exercises should be followed by high-speed exercises with light resistance. Once sufficient ROM and strength have been regained, proprioceptive exercises may be integrated.[14]
- Operative treatment
To restore the anatomical structures with sufficient strength, passive and active training of the assisted ROM are needed. Most patients lose some motion and do not recover entirely.
Postsurgical rehabilitation for this injury varies according to which ligaments were injured and repaired. Initially, a brace with limits of 40° of extension and 70° of flexion should be worn if a continuous passive-motion machine is used. From the start, quadriceps settings are performed in order to increase quadriceps control. In the first postoperative week it's also very important to work on full extension. This can be achieved by doing therapeutic exercises. From weeks 7 to 10, ROM therapy can begin, stressing full extension and flexion. After weeks 11 to 24, the patient should have regained full flexion and extension and strength training can begin using closed kinetic chain exercises (squats, light leg presses,..). Strength training continues through weeks 25 to 36 but becomes more advanced. After the patient has reestablished bulk and strength around the knee, proprioceptive exercises are integrated. After week 37 the patient can return to sports and heavy work, provided that he or she has passed functional tests.[8]
Prognosis[edit | edit source]
A patient with a knee dislocation is faced with a long rehabilitation program, with return to full activity taking at least 9 to 12 months. Most of the knee dislocations require reconstruction surgery. That is because major injury to the artery occurs in 21%-32% of all knee dislocations and because of the severe ligament injury. After the treatment and surgery the results are good. In most cases the damaged knees return to an almost normal state. Chronic pain is a common problem, occurring in 46% of cases. The prognosis is best with an optimal rehabilitation exercise program.[15]
Resources
[edit | edit source]
Web MD, Knee pain health center. http://www.webmd.com/pain-management/knee-pain/knee-dislocation (assessed 14 april 2011)
Henrichs A. A review of knee dislocations. Journal of Athletic Training 2004;39(4): 365–369
Rihn J, Groff Y, Harner C & Cha P. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004 Sep-Oct;12(5): 334-46.
Levy B, Peskun C, Fanelli G, Stannard J, Stuart M, MacDonald P, Marx R, Boyd J & Whelan D. Diagnosis and management of knee dislocations. Phys Sportsmed. 2010 Dec;38(4): 101-11.
Clinical Bottom Line[edit | edit source]
add text here
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Brautigan B, Johnson DL. The epidemiology of knee dislocations. Clinics in sports medicine 2000;19(3):387-97.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee. Injury 2011;42(11):1198-204.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Robertson A, Nutton RW, Keating JF. Dislocation of the knee. The Journal of bone and joint surgery. British volume 2006;88(6):706-11.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Fanelli GC, editor. The multiple ligament injured knee: A practical guide to management. New York: Springer Science, 2004.
- ↑ 5.0 5.1 Flint L, Meredith JW, Schwab CW. Trauma: contemporary principles and therapy. Philadelphia; 2008.
- ↑ 6.0 6.1 LCDR Damon Shearer, DO; Laurie Lomasney, MD; Kenneth Pierce, MD. Dislocation of the knee: imaging findings, J Spec Oper Med. 2010 Winter;10(1):43-7. Level of evidence: A1
- ↑ Rihn J, Groff Y, Harner C & Cha P. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004 Sep-Oct;12(5): 334-46. A1
- ↑ 8.0 8.1 8.2 8.3 8.4 Henrichs A. A review of knee dislocations. Journal of Athletic Training 2004;39(4):365–369.
- ↑ R. Schenck Jr. MD „Classification of knee dislocations” Operative Techniques in Sports Medicine, Vol 11, No 3 (July), 2003) Level of evidence 2A
- ↑ 10.0 10.1 Levy B, Peskun C, Fanelli G, Stannard J, Stuart M, MacDonald P, Marx R, Boyd J & Whelan D. Diagnosis and management of knee dislocations. Phys Sportsmed. 2010 Dec;38(4): 101-11. A1
- ↑ 11.0 11.1 11.2 11.3 Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.
- ↑ Demirag, B. et al, Knee dislocations: an evaluation of surgical and conservative treatment, Turkish Journal of Trauma & Emergency Surgery Ulus Travma Derg 2004;10(4):239-244:Grade of recommendation: B
- ↑ Chun-Chien Cheng; Jih-Yang Ko. Early Reduction for Congenital Dislocation of the Knee within Twenty-four Hours of Birth. Chang Gung Med J 2010;33:266-73. Grade of recommendation: C
- ↑ John M. Siliski et co, traumatic disorders of the knee. Grade of recommendation: B.
- ↑ William C. Shiel Jr., MD, FACP, FACR ; “Knee Dislocation”, http://www.emedicinehealth.com/knee_dislocation/fckLRpage10_em.htm#prognosis_of_knee_dislocation, bezocht op 6/11/13. Grade of recommandation: C.