Pes Anserinus Bursitis: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Prepatellar bursitis" to "[[Prepatellar Bursitis") |
||
| (48 intermediate revisions by 12 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors ''' | '''Original Editors ''' - [[User:Glenn Demeyer|Glenn Demeyer]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Definition/Description == | ||
Pes Anserine [http://www.physio-pedia.com/index.php5?title=Bursitis bursitis], also known as intertendinous bursa, is an inflammatory condition of bursa of the conjoined insertion of the sartorius, gracilis and semitendinosus<ref name="Rennie">Rennie WJ, Saifuddin A. Pes anserine bursitis: Incidence in symptomatic knees and clinical presentation. Skeletal Radiol. 2005;34:395–8.</ref>. We can locate this at the proximal medial aspect of the [[Knee]], two inches below the medial knee joint line between the pes anserinus tendons<ref name="Moschowitz">Moschowitz E. Bursitis of the sartorius bursa: an undescribed malady simulating chronic arthritis. JAMA 1937; 109:1362</ref><ref name="Huang">Huang TW, Wang CJ, Huang SC. Polyethylene-induced pes anserinus bursitis mimicking an infected total knee arthroplasty: a case report and review of the literature. J Arthroplasty. 2003 Apr;18(3):383-6.</ref><ref name="Osman">Osman MK, Irwin GJ, Huntley JS.Swelling around a child's knee. Clin Anat. 2011 Oct;24(7):914-7.</ref>. | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
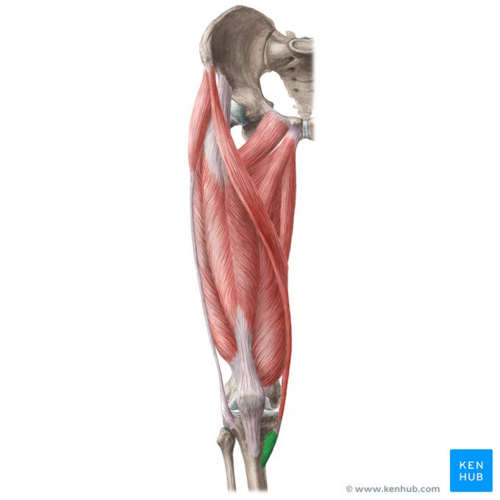
[[File:Pes anserinus - Kenhub.png|alt=Pes anserinus (highlighted in green) - anterior view|right|frameless|500x500px|Pes anserinus (highlighted in green) - anterior view]] | |||
The Pes Anserine bursa is a fluid filled vesicle. It secretes synovial fluid in order to reduce friction between tissues, and also works as a cushion for bones, tendons and muscles<ref name="Tschirch">Tschirch FTC, Schmid MR, Pfirrmann CWA, et al. Prevalence and size of meniscal cysts, ganglionic cysts, synovial cysts of the popliteal space, fluid filled bursae, and other fluid filled collections in asymptomatic knees on MR imaging. AJR Am J Roentgenol 2003; 180:1431–1436.</ref>. The inflammation of the bursa does not appear suddenly, but rather progresses over a period of time. [[Bursitis]] can also occur in the [[Shoulder Bursitis|shoulder]], [[Prepatellar Bursitis|knee]], [[Iliopsoas Bursitis|hip]], [[Olecranon Bursitis|elbow]] and big toe. <br> | |||
The Pes Anserine, also called the ‘Goose Foot’ is the insertion of the [[sartorius]], [[gracilis]] and [[semitendinosus]] muscles, which are conjoined proximally on the medial side of the [[Tibia]]. The three tendons of the Pes Anserine are located superficial to the medial collateral ligament (MCL) of the knee<ref name="Wood">Wood LR, Peat G, Thomas E, et al. The contribution of selected non-articular conditions to knee pain severity and associated disability in older adults. Osteoarthritis Cartilage. Jun 2008;16(6):647-53.</ref>. The sartorius and gracilis muscles are adductors of the leg (i.e. they pull the leg towards the median axis of the body). The semitendinosus muscle is part of the hamstrings muscle group located at the back of your upper leg. Together, these three muscles are primarily flexors of the knee and internal rotators<ref name="Miller">Miller RH III. Knee injuries. In: Canale ST, ed. Campbell's operative orthopaedics. St Louis: Mosby; 1998: 1113-1299.</ref>. | |||
Image: Pes anserinus (highlighted in green) - anterior view<ref >Pes anserinus (highlighted in green) - anterior view image - © Kenhub https://www.kenhub.com/en/library/anatomy/lower-leg-and-knee-anatomy</ref> <br> | |||
== Epidemiology/Etiology == | |||
== | Pes Anserine bursitis often occurs when the related muscles are repeatedly used, by doing movements such as flexion and adduction. This causes friction and also increases pressure on the bursa. The bursitis can also be due to a trauma, such as a direct hit in the Pes Anserine region. A contusion to this area results in an increased release of synovial fluid in the lining of the bursa. The bursa then becomes inflamed and tendered or painful <ref name="Huang" /> and underlying [[Osteoarthritis]] of the [[Knee Osteoarthritis|knee]]<ref name="Stuttle">Stuttle FL. The no-name and no-fame bursa. Clin Orthop 1959; 15:197-199.</ref>. | ||
Reports suggest that anserine bursitis is more common in overweight middle-aged females. We can explain this by the fact that women have a wider pelvis, resulting in angulation of the knee in the frontal plane, which leads to more pressure in the area of insertion of the pes anserinus by genu valgum<ref name="Helfenstein">Helfenstein M Jr, Kuromoto J. Anserine syndrome. Rev Bras Reumatol. 2010 May-Jun;50(3):313-27.</ref>. | |||
We can say that an inflamed bursa is not a primary pathology, but rather a consequence of an earlier complication. | |||
== | == Characteristics/Clinical Presentation == | ||
Pes Anserine bursitis causes pain on the inside of the knee (mostly during running or taking stairs). The patient may experience spontaneous anteromedial knee pain on climbing or descending stairs and tenderness at the PA <ref name="Huang" /><ref name="Rennie" /><ref name="Glencross" />. As well, the region around the bursa will be swollen or tender to touch<ref name="Forbes">Forbes JR, Helms CA, Janzen DL. Acute pes anserine bursitis: MR imaging. Radiology 1995; 194:525-527.</ref>. | |||
Other clinical presentations may include: | |||
*Decreased muscle strength | |||
*Gait deviations | |||
*Decreased function | |||
*Decreased ROM | |||
*Postural dysfunction/impaired lower extremity biomechanics | |||
Aggravating factors include activities that require movements like flexion and endorotation, as well as exorotation and adduction. Pivoting, kicking, squatting or quick movements from side to side, such as in the sports mentioned above, may also cause further irritation. | |||
== Differential Diagnosis == | |||
Pes Anserine bursitis is often confused with other causes of medial knee pain<ref name="Safran">Safran MR, Fu FH. Uncommon causes of knee pain in the athlete. Orthop Clin North Am 1995; 26:547-549.</ref><ref name="Matsumoto">Matsumoto K, Sinusuke H, Ogata M. Juxta-articular bone cysts at the insertion of the pes anserinus. J Bone Joint Surg 1990; 72A:286-290.</ref><ref name="Hennigan">Hennigan SP, Schenck CD, Mesgarzadeh M et al. The semimembranosus- tibial collateral ligament bursa. Anatomical study and magnetic resonance imaging. J Bone Joint Surg 1994; 76A:1322-1327.</ref><ref name="Kerlan">Kerlan RK, Glousman RE. Tibial collateral ligament bursitis. Am J Sports Med 1988; 16:344-346.</ref>: | |||
== | *[[Leg and Foot Stress Fractures|Stress-fracture]] of the shin bone on the proximedial side will cause pain in the area of the Pes Anserine. | ||
*[[Patellofemoral Pain Syndrome|Patellofemoral syndrome]] | |||
*[[Medial Collateral Ligament Injury of the Knee|Medial meniscus lesion]] and [[Osteoarthritis|osteoarthritis]]: Pain and sensitivity would be present in the medial compartment, while in the pes anserinus bursitis they are located inferomedial to the medial joint interline. Stress maneuvers of the medial collateral ligament, with or without instability, may contribute to the diagnosis of lesions of the medial collateral ligament<ref name="Uson">Uson J, et al. Pes anserinus tendino-bursitis: what are we talking about? Scand J Rheumatol. 2000;29(3):184-6.</ref><ref name="Helfenstein" />. | |||
*Knee pain secondary to L3-L4 [[Lumbar Radiculopathy|radiculopathy]] is associated with lumbar pain without pain on digital pressure of the anserine region<ref name="Helfenstein" />. | |||
*Panniculitis<ref name="Glencross">Glencross PM. Medscape: Pes Anserine Bursitis. www.emedicine.medscape.com/article/308694-diagnosis (accessed 26 December 2013).</ref> occurs in obese individuals, and causes painful inflammation of subcutaneous fat at night. | |||
*Semimembranosus tendinitis will often occur as a running injury. | |||
*Medial [[Plica Syndrome]], which can cause pain and tenderness on the medial side of the knee. | |||
*Extra-articular cystic lesions: synovial cyst, ganglionic cyst, parameniscal cyst, pigmented villonodular synovitis, synovial sarcoma<ref name="Huang" /> | |||
*In addition to the conditions listed above, other problems to be considered include the following<ref name="Rennie" />: | |||
**Atypical medial meniscal cysts | |||
**Juxta-articular bone cysts | |||
**Semimembranosus bursitis | |||
**Tibial collateral ligament bursitis | |||
== Diagnostic Procedures == | |||
== | Lateral x-ray views of the patient's knee are very useful for ruling out a stress fracture, arthritis or even [[Osteochondritis Dissecans of the Knee|Osteochondritis Dissecans]]. An MRI is needed to clarify damage caused to other regions of the medial side of the knee. An MRI could prevent unnecessary arthroscopy. MRI findings should be compared with those of a physical examination<ref name="Zeiss">Zeiss J, Coombs R, Booth R, Saddemi S. Chronic bursitis presenting as a mass in the pes anserine bursa: MR diagnosis. J Comput Assist Tomogr 1993; 17:137-140.</ref><ref name="Hall">Hall FM, Joffe N. CT imaging of the anserine bursa. AJR Am J Roentgenol 1988; 150:1107-1108.</ref>. Sinography (radiography of a sinus following the injection of a radiopaque medium) is the best method for establishing the diagnosis when other imaging modalities, including MRI and CT, are not feasible<ref name="Huang" />. A Lidocaine/Corticosteriod injection in the area of the bursa which will help determine the contribution of this pathology to the patient's overall knee pain. | ||
== Outcome Measures == | |||
*[[Lower Extremity Functional Scale (LEFS)]] <br> | |||
See [[Outcome Measures|Outcome Measures Database]] for more. | |||
== | == Examination == | ||
The pes anserine bursa can be palpated at a point slightly distal to the tibial tubercle and about 3-4 cm medial to it (about 2 fingerbreadths)<ref name="Glencross" />. | |||
{{#ev:youtube|MtqHdqAdllU|300}} | |||
Examine hamstring length with the patient in the supine position. Bend the patient's hip 90° and then extend the knee as far as possible. How far the knee can be extended will indicate hamstring length and tightness. If the patient's knee can be straightened completely than the hamstrings are not tight.<br> | |||
{{#ev:youtube|pi6tiTKGO0M|300}} | |||
<br>With the sports-related variant of pes anserine bursitis, symptoms may be reproduced by means of resisted internal rotation and resisted flexion of the knee. With the chronic variant in older adults, flexion or extension of the knee usually does not elicit pain<ref name="Glencross" />. | |||
== | == Medical Management == | ||
The initial treatment of pes anserinus bursitis should include relative rest of the affected knee and non-steroidal anti-inflammatory drugs (NSAID)<ref name="Rennie" />. Additional modalities, including local injection of a corticoid such as methylprednisolone, are indicated is some cases. Intrabursal injection of local anesthetics, corticosteroids, or both constitutes a second line of treatment<ref name="Rennie" />. Surgical treatment is indicated in cases with failure to conservative treatments. Simple incision and drainage of the distended bursa can improve symptoms in some reported cases<ref name="Huang" /><ref name="Rennie" />. The bursa may be removed if chronic infection cannot be cleared up with antibiotics. After surgery, if the bursa is removed, follow the same steps of rehabilitation and recovery outlined under physical therapy management<ref name="Helfenstein" />. If the bursitis becomes infected and standard antibiotic treatments are ineffective, A surgical decompression of the bursa may be a solution in this case. <br> | |||
< | |||
< | |||
< | |||
== Physical Therapy Management == | |||
< | Physiotherapy is the mainstay in the treatment of the Pes Anserine syndrome. To temper the pain caused by the bursitis, the most important thing of all is rest. Avoid stairs, climbing, or other irritating activities to quiet down the bursa and the related pain<ref name="Rennie" />. Nonsteroidal anti-inflammatory drugs (NSAID) can be taken to alleviate the pain. Restrict movement and alternately apply [[Cryotherapy|ice]] during the inflammatory phase. An ice massage of 15 minutes every 4-7 hours will reduce the inflammation. An elastic bandage can be wrapped around the knee to reduce any swelling or to prevent swelling from occurring<ref name="Rennie" />. Be careful not to increase friction. Teach the patient muscle-conditioning exercises<ref name="O'Donoghue">O'Donoghue DH. Injuries of the knee. In: O'Donoghue DH, ed. Treatment of injuries to athletes, 4th edn. Philadelphia: Saunders; 1987: 470-471.</ref>. These may include leg stretching exercises such as hamstring stretch, standing calf stretch, standing quadriceps stretch, hip adductor stretch, heel slide, quadriceps isometrics, hamstrings isometrics<ref name="Rennie" />. Progression of these exercises may involve [[Closed Chain Exercise|closed-kinetic chain exercises]] such as single-knee dips, squats and leg presses. Resisted leg-pulls using elastic tubing are also included. | ||
[[ | The [[Closed Chain Exercise|closed-kinetic chain exercises]] are also a recommended method to prevent the development of collateral knee instability, which occurs to be a risk factor of Pes Anserine bursitis.<ref>Alvarez-Nemegyei, José. "Risk factors for pes anserinus tendinitis/bursitis syndrome: a case control study." ''JCR: Journal of Clinical Rheumatology'' 13.2 (2007): 63-65.</ref><br> | ||
{{#ev:youtube|kdJIsgWbh8s|300}} | |||
[[Therapeutic Ultrasound|Ultrasound]] has been documented as effective in the reduction of the inflammatory process in pes anserine bursitis.<ref name="Helfenstein" /> Some patients receive an injection which consists of a solution of anesthetic and steroid. Afterwards, a physiotherapist will give a hamstring stretching program and a concurrent closed-chain quadriceps strengthening program that has to repeated several times a day. This will result in less pain at about 6-8 weeks.<br> | |||
Kinesiotaping is more effective than naproxen or physical therapy in reduction of pain and swelling.<ref>Homayouni, Kaynoosh, Shima Foruzi, and Fereshte Kalhori. "Effects of kinesiotaping versus non-steroidal anti-inflammatory drugs and physical therapy for treatment of pes anserinus tendino-bursitis: A randomized comparative clinical trial." ''The Physician and sportsmedicine'' 44.3 (2016): 252-256.</ref> | |||
== Clinical Bottom Line == | |||
Pes anserine bursitis is commonly associated with osteoarthritis and/or overweight females. A typical characteristic is spontaneous anteromedial knee pain on climbing or descending stairs. The differential diagnosis is very encompassing. It does not disappear without treatment such as rest, ice application, stretching and ultrasound. Another frequently used treatment is intrabursal injection of corticosteroids. <br> | |||
< | == References == | ||
<references /><br> | |||
[[Category:Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Knee]] | |||
[[Category:Conditions]] | |||
[[Category:Knee - Conditions]] | |||
[[Category:Primary Contact]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Bursitis]] | |||
Latest revision as of 15:34, 19 October 2023
Original Editors - Glenn Demeyer
Top Contributors - Admin, Stefanie Van De Vijver, Glenn Demeyer, Kim Jackson, Daphne Jackson, Laure Leyers, Wanda van Niekerk, Rachael Lowe, WikiSysop, Phaedra Plas, Candace Goh, Joao Costa, 127.0.0.1, Celine De Wolf, Claire Knott and Hamelryck Sascha
Definition/Description[edit | edit source]
Pes Anserine bursitis, also known as intertendinous bursa, is an inflammatory condition of bursa of the conjoined insertion of the sartorius, gracilis and semitendinosus[1]. We can locate this at the proximal medial aspect of the Knee, two inches below the medial knee joint line between the pes anserinus tendons[2][3][4].
Clinically Relevant Anatomy[edit | edit source]
The Pes Anserine bursa is a fluid filled vesicle. It secretes synovial fluid in order to reduce friction between tissues, and also works as a cushion for bones, tendons and muscles[5]. The inflammation of the bursa does not appear suddenly, but rather progresses over a period of time. Bursitis can also occur in the shoulder, knee, hip, elbow and big toe.
The Pes Anserine, also called the ‘Goose Foot’ is the insertion of the sartorius, gracilis and semitendinosus muscles, which are conjoined proximally on the medial side of the Tibia. The three tendons of the Pes Anserine are located superficial to the medial collateral ligament (MCL) of the knee[6]. The sartorius and gracilis muscles are adductors of the leg (i.e. they pull the leg towards the median axis of the body). The semitendinosus muscle is part of the hamstrings muscle group located at the back of your upper leg. Together, these three muscles are primarily flexors of the knee and internal rotators[7].
Image: Pes anserinus (highlighted in green) - anterior view[8]
Epidemiology/Etiology[edit | edit source]
Pes Anserine bursitis often occurs when the related muscles are repeatedly used, by doing movements such as flexion and adduction. This causes friction and also increases pressure on the bursa. The bursitis can also be due to a trauma, such as a direct hit in the Pes Anserine region. A contusion to this area results in an increased release of synovial fluid in the lining of the bursa. The bursa then becomes inflamed and tendered or painful [3] and underlying Osteoarthritis of the knee[9].
Reports suggest that anserine bursitis is more common in overweight middle-aged females. We can explain this by the fact that women have a wider pelvis, resulting in angulation of the knee in the frontal plane, which leads to more pressure in the area of insertion of the pes anserinus by genu valgum[10].
We can say that an inflamed bursa is not a primary pathology, but rather a consequence of an earlier complication.
Characteristics/Clinical Presentation[edit | edit source]
Pes Anserine bursitis causes pain on the inside of the knee (mostly during running or taking stairs). The patient may experience spontaneous anteromedial knee pain on climbing or descending stairs and tenderness at the PA [3][1][11]. As well, the region around the bursa will be swollen or tender to touch[12].
Other clinical presentations may include:
- Decreased muscle strength
- Gait deviations
- Decreased function
- Decreased ROM
- Postural dysfunction/impaired lower extremity biomechanics
Aggravating factors include activities that require movements like flexion and endorotation, as well as exorotation and adduction. Pivoting, kicking, squatting or quick movements from side to side, such as in the sports mentioned above, may also cause further irritation.
Differential Diagnosis[edit | edit source]
Pes Anserine bursitis is often confused with other causes of medial knee pain[13][14][15][16]:
- Stress-fracture of the shin bone on the proximedial side will cause pain in the area of the Pes Anserine.
- Patellofemoral syndrome
- Medial meniscus lesion and osteoarthritis: Pain and sensitivity would be present in the medial compartment, while in the pes anserinus bursitis they are located inferomedial to the medial joint interline. Stress maneuvers of the medial collateral ligament, with or without instability, may contribute to the diagnosis of lesions of the medial collateral ligament[17][10].
- Knee pain secondary to L3-L4 radiculopathy is associated with lumbar pain without pain on digital pressure of the anserine region[10].
- Panniculitis[11] occurs in obese individuals, and causes painful inflammation of subcutaneous fat at night.
- Semimembranosus tendinitis will often occur as a running injury.
- Medial Plica Syndrome, which can cause pain and tenderness on the medial side of the knee.
- Extra-articular cystic lesions: synovial cyst, ganglionic cyst, parameniscal cyst, pigmented villonodular synovitis, synovial sarcoma[3]
- In addition to the conditions listed above, other problems to be considered include the following[1]:
- Atypical medial meniscal cysts
- Juxta-articular bone cysts
- Semimembranosus bursitis
- Tibial collateral ligament bursitis
Diagnostic Procedures[edit | edit source]
Lateral x-ray views of the patient's knee are very useful for ruling out a stress fracture, arthritis or even Osteochondritis Dissecans. An MRI is needed to clarify damage caused to other regions of the medial side of the knee. An MRI could prevent unnecessary arthroscopy. MRI findings should be compared with those of a physical examination[18][19]. Sinography (radiography of a sinus following the injection of a radiopaque medium) is the best method for establishing the diagnosis when other imaging modalities, including MRI and CT, are not feasible[3]. A Lidocaine/Corticosteriod injection in the area of the bursa which will help determine the contribution of this pathology to the patient's overall knee pain.
Outcome Measures[edit | edit source]
See Outcome Measures Database for more.
Examination[edit | edit source]
The pes anserine bursa can be palpated at a point slightly distal to the tibial tubercle and about 3-4 cm medial to it (about 2 fingerbreadths)[11].
Examine hamstring length with the patient in the supine position. Bend the patient's hip 90° and then extend the knee as far as possible. How far the knee can be extended will indicate hamstring length and tightness. If the patient's knee can be straightened completely than the hamstrings are not tight.
With the sports-related variant of pes anserine bursitis, symptoms may be reproduced by means of resisted internal rotation and resisted flexion of the knee. With the chronic variant in older adults, flexion or extension of the knee usually does not elicit pain[11].
Medical Management[edit | edit source]
The initial treatment of pes anserinus bursitis should include relative rest of the affected knee and non-steroidal anti-inflammatory drugs (NSAID)[1]. Additional modalities, including local injection of a corticoid such as methylprednisolone, are indicated is some cases. Intrabursal injection of local anesthetics, corticosteroids, or both constitutes a second line of treatment[1]. Surgical treatment is indicated in cases with failure to conservative treatments. Simple incision and drainage of the distended bursa can improve symptoms in some reported cases[3][1]. The bursa may be removed if chronic infection cannot be cleared up with antibiotics. After surgery, if the bursa is removed, follow the same steps of rehabilitation and recovery outlined under physical therapy management[10]. If the bursitis becomes infected and standard antibiotic treatments are ineffective, A surgical decompression of the bursa may be a solution in this case.
Physical Therapy Management[edit | edit source]
Physiotherapy is the mainstay in the treatment of the Pes Anserine syndrome. To temper the pain caused by the bursitis, the most important thing of all is rest. Avoid stairs, climbing, or other irritating activities to quiet down the bursa and the related pain[1]. Nonsteroidal anti-inflammatory drugs (NSAID) can be taken to alleviate the pain. Restrict movement and alternately apply ice during the inflammatory phase. An ice massage of 15 minutes every 4-7 hours will reduce the inflammation. An elastic bandage can be wrapped around the knee to reduce any swelling or to prevent swelling from occurring[1]. Be careful not to increase friction. Teach the patient muscle-conditioning exercises[20]. These may include leg stretching exercises such as hamstring stretch, standing calf stretch, standing quadriceps stretch, hip adductor stretch, heel slide, quadriceps isometrics, hamstrings isometrics[1]. Progression of these exercises may involve closed-kinetic chain exercises such as single-knee dips, squats and leg presses. Resisted leg-pulls using elastic tubing are also included.
The closed-kinetic chain exercises are also a recommended method to prevent the development of collateral knee instability, which occurs to be a risk factor of Pes Anserine bursitis.[21]
Ultrasound has been documented as effective in the reduction of the inflammatory process in pes anserine bursitis.[10] Some patients receive an injection which consists of a solution of anesthetic and steroid. Afterwards, a physiotherapist will give a hamstring stretching program and a concurrent closed-chain quadriceps strengthening program that has to repeated several times a day. This will result in less pain at about 6-8 weeks.
Kinesiotaping is more effective than naproxen or physical therapy in reduction of pain and swelling.[22]
Clinical Bottom Line[edit | edit source]
Pes anserine bursitis is commonly associated with osteoarthritis and/or overweight females. A typical characteristic is spontaneous anteromedial knee pain on climbing or descending stairs. The differential diagnosis is very encompassing. It does not disappear without treatment such as rest, ice application, stretching and ultrasound. Another frequently used treatment is intrabursal injection of corticosteroids.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Rennie WJ, Saifuddin A. Pes anserine bursitis: Incidence in symptomatic knees and clinical presentation. Skeletal Radiol. 2005;34:395–8.
- ↑ Moschowitz E. Bursitis of the sartorius bursa: an undescribed malady simulating chronic arthritis. JAMA 1937; 109:1362
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Huang TW, Wang CJ, Huang SC. Polyethylene-induced pes anserinus bursitis mimicking an infected total knee arthroplasty: a case report and review of the literature. J Arthroplasty. 2003 Apr;18(3):383-6.
- ↑ Osman MK, Irwin GJ, Huntley JS.Swelling around a child's knee. Clin Anat. 2011 Oct;24(7):914-7.
- ↑ Tschirch FTC, Schmid MR, Pfirrmann CWA, et al. Prevalence and size of meniscal cysts, ganglionic cysts, synovial cysts of the popliteal space, fluid filled bursae, and other fluid filled collections in asymptomatic knees on MR imaging. AJR Am J Roentgenol 2003; 180:1431–1436.
- ↑ Wood LR, Peat G, Thomas E, et al. The contribution of selected non-articular conditions to knee pain severity and associated disability in older adults. Osteoarthritis Cartilage. Jun 2008;16(6):647-53.
- ↑ Miller RH III. Knee injuries. In: Canale ST, ed. Campbell's operative orthopaedics. St Louis: Mosby; 1998: 1113-1299.
- ↑ Pes anserinus (highlighted in green) - anterior view image - © Kenhub https://www.kenhub.com/en/library/anatomy/lower-leg-and-knee-anatomy
- ↑ Stuttle FL. The no-name and no-fame bursa. Clin Orthop 1959; 15:197-199.
- ↑ 10.0 10.1 10.2 10.3 10.4 Helfenstein M Jr, Kuromoto J. Anserine syndrome. Rev Bras Reumatol. 2010 May-Jun;50(3):313-27.
- ↑ 11.0 11.1 11.2 11.3 Glencross PM. Medscape: Pes Anserine Bursitis. www.emedicine.medscape.com/article/308694-diagnosis (accessed 26 December 2013).
- ↑ Forbes JR, Helms CA, Janzen DL. Acute pes anserine bursitis: MR imaging. Radiology 1995; 194:525-527.
- ↑ Safran MR, Fu FH. Uncommon causes of knee pain in the athlete. Orthop Clin North Am 1995; 26:547-549.
- ↑ Matsumoto K, Sinusuke H, Ogata M. Juxta-articular bone cysts at the insertion of the pes anserinus. J Bone Joint Surg 1990; 72A:286-290.
- ↑ Hennigan SP, Schenck CD, Mesgarzadeh M et al. The semimembranosus- tibial collateral ligament bursa. Anatomical study and magnetic resonance imaging. J Bone Joint Surg 1994; 76A:1322-1327.
- ↑ Kerlan RK, Glousman RE. Tibial collateral ligament bursitis. Am J Sports Med 1988; 16:344-346.
- ↑ Uson J, et al. Pes anserinus tendino-bursitis: what are we talking about? Scand J Rheumatol. 2000;29(3):184-6.
- ↑ Zeiss J, Coombs R, Booth R, Saddemi S. Chronic bursitis presenting as a mass in the pes anserine bursa: MR diagnosis. J Comput Assist Tomogr 1993; 17:137-140.
- ↑ Hall FM, Joffe N. CT imaging of the anserine bursa. AJR Am J Roentgenol 1988; 150:1107-1108.
- ↑ O'Donoghue DH. Injuries of the knee. In: O'Donoghue DH, ed. Treatment of injuries to athletes, 4th edn. Philadelphia: Saunders; 1987: 470-471.
- ↑ Alvarez-Nemegyei, José. "Risk factors for pes anserinus tendinitis/bursitis syndrome: a case control study." JCR: Journal of Clinical Rheumatology 13.2 (2007): 63-65.
- ↑ Homayouni, Kaynoosh, Shima Foruzi, and Fereshte Kalhori. "Effects of kinesiotaping versus non-steroidal anti-inflammatory drugs and physical therapy for treatment of pes anserinus tendino-bursitis: A randomized comparative clinical trial." The Physician and sportsmedicine 44.3 (2016): 252-256.