Anterior Shoulder Instability: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (33 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> '''Original Editor '''- [[User:Liesbeth De Feyter|Liesbeth De Feyter]], [[User:Daphné Bertrand|Daphné Bertrand]], [[User:Lisa De Pelsemaeker|Lisa De Pelsemaeker]], [[User:Arnaud Jacquet|Arnaud Jacquet]] as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel Evidence-Based Practice Project]] | ||
'''Original | |||
'''Top Contributors''' - | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Definition == | |||
The term ''anterior shoulder instability'' refers to a [[shoulder]] in which soft tissue or bony insult allows the humeral head to sublux or dislocate from the glenoid fossa.<ref>Medscape. Anterior Glenohumeral Instability. Available from: https://emedicine.medscape.com/article/1262004-overview (accessed 29 August 2020).</ref> It is an injury to the [[Glenohumeral Joint|glenohumeral joint]] (GHJ) where the [[humerus]] is displaced from its normal position in the center of the glenoid fossa and the joint surfaces no longer touch each other. | |||
Also see related pages for [[Shoulder Instability|shoulder instability]], [[Shoulder Subluxation]] and [[Shoulder Dislocation|shoulder dislocation]]. | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
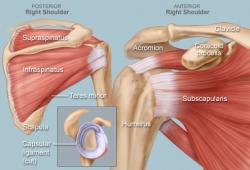
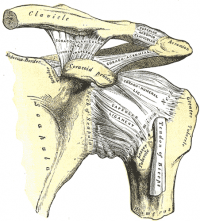
The glenohumeral joint (multi-axial spheroidal joint) is one of the largest and most complex joints in the body. It has the greatest range of movement of any joint, but this leaves it inherently | The [[Glenohumeral Joint|glenohumeral joint]] (multi-axial spheroidal joint) is one of the largest and most complex joints in the body. It has the greatest range of movement of any joint, but this leaves it inherently unstable and with the highest chance of dislocation of all the body's joints. The GHJ is formed where the humeral head fits into the glenoid fossa, an irregular oval shape, which is an extension of the [[scapula]], like a ball and socket, although only 25% of the humeral head makes contact with the glenoid fossa at any time. | ||
* The acromion: a bony projection off the scapula | |||
* The clavicle: which joins the acromion via the acromioclavicular joint and distal sternoclavicular joint to the axial skeleton | This joint is surrounded by numerous [[Ligament|ligaments]] and [[Muscle|muscles]] which give it stability. The surrounding capsule may also add some stability with the coracohumeral and glenohumeral ligaments reinforcing the capsule. Other important [[Bone|bones]] in the shoulder include: | ||
* The coracoid process: a hook-like bony projection from the scapula | * The acromion: a bony projection off the [[scapula]] | ||
* The [[Clavicula|clavicle]]: which joins the acromion via the [[Acromioclavicular Joint|acromioclavicular joint]] and distal [[Sternoclavicular Joint|sternoclavicular joint]] to the axial skeleton | |||
* The coracoid process: a hook-like bony projection from the [[scapula]] | |||
The shoulder has several other important structures: | The shoulder has several other important structures: | ||
* The rotator cuff | * The [[Rotator Cuff|rotator cuff]]: A collection of 4 muscles originating from the [[scapula]] ([[supraspinatus]], [[infraspinatus]], [[subscapularis]] and [[Teres Minor|teres minor]]) which stabilise the GHJ and allow the wide range of motion. | ||
* The bursae: | * The bursae: There are a number of bursae associated with the [[shoulder]] of which the subacromial bursa is the one most likely to become symptomatic with [[Shoulder Bursitis|bursitis]]. It sits between the superior surface of the [[supraspinatus]] tendon and the acromium, coracoid an the coracoacromial ligament, extending down over the humeral tendinous attachment of [[supraspinatus]] | ||
* The labrum: | * The [[Glenoid Labrum|labrum]]: A fibrous ring of cartilage which extends up from the glenoid providing stability in the form of a deeper cup for the humeral head to fit into.<ref>Web MD. Picture of the shoulder. Available from: http://www.webmd.com/pain-management/picture-of-the-shoulder (accessed 29 August 2020).</ref> | ||
[[Image:123.jpg|250x250px]] | [[Image:123.jpg|250x250px]] | ||
| Line 26: | Line 28: | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
<u> | === Epidemiology === | ||
<u><br></u>Anterior [[Shoulder Dislocation|shoulder dislocations]] are much more common than posterior dislocations.<ref name="Andrew et al" /> | |||
< | Research suggests that incidence of recurrent [[Shoulder Dislocation|shoulder dislocation]] is significantly higher in younger patients.<ref name="Arash et al">Araghi A, Prasarn M, St Clair S, Zuckerman JD. [http://presentationgrafix.com/_dev/cake/files/archive/pdfs/643.pdf Recurrent anterior glenohumeral instability with onset after forty years of age.] Bull Hosp Joint Dis 2005 Jan 1;62:99-101.</ref><ref name="E et al" /> The consequences of an initial anterior glenohumeral dislocation in patients over forty years of age are quite different than in the younger population, primarily due to the increased incidence of [[Rotator Cuff Tears|rotator cuff tears]] and associated neurovascular injuries. The anterior or posterior supporting structures of the [[shoulder]] can also be disrupted following an anterior dislocation. In the younger population, anterior capsuloligamentous structures most commonly fail, whereas in older patients with pre-existing degenerative weakening of the [[Rotator Cuff|rotator cuff]], the posterior structures are more likely to fail.<ref name="Arash et al" /><br> | ||
=== Etiology === | |||
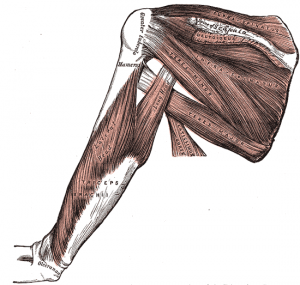
The GHJ is stabilised by both dynamic and static structures.<ref name="Arash et al" />[[Image:Rotator cuff muscles.png|thumb|right|300px|Rotator Cuff Muscles]] | |||
[[ | *Dynamic stabilisers: [[Rotator Cuff|Rotator cuff muscles]], [[Biceps Brachii]], [[deltoid]] | ||
*Static stabilisers: Glenohumeral joint capsule, the glenohumeral ligaments, the [[Glenoid Labrum|labrum]], negative pressure within the joint capsule, and the bony congruity of the joint.<ref name="Andrew et al">Chen AL, Bosco III JA. [https://go.gale.com/ps/anonymous?id=GALE%7CA166094301&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=19369719&p=HRCA&sw=w Glenohumeral bone loss and anterior instability.] Bulletin of the NYU hospital for joint diseases 2006 Dec 22;64(3-4):130-138.</ref><ref name="E et al" /> | |||
*The [[Glenoid Labrum|labrum]]: This concave compression mechanism plays an important role in the stability of the glenohumeral joint by maintaining the localisation of the humeral head at the glenoid against translational forces. The glenoid concavity is established by the glenoid shape, the glenoid cartilage and the glenoid labrum. The glenoid labrum increases the width and depth of the glenoid. Instability is increased with the size of the glenoid defect.<ref name="Yong et al">Rhee YG, Lim CT. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2266647/ Glenoid defect associated with anterior shoulder instability: results of open Bankart repair.] Int Orthop 2007;31(5):629-34.</ref> | |||
*Static stabilisers: | *The glenohumeral ligaments: The superior glenohumeral ligament functions primarily to resist inferior translation and external rotation of the humeral head in the adducted arm. The middle glenohumeral ligament functions primarily to resist external rotation from 0° to 90° and provides anterior stability to the moderately abducted shoulder. The inferior glenohumeral ligament is composed of two bands, anterior and posterior, and the intervening capsule. The primary function of the anterior band is to resist anteroinferior translation.<ref name="E et al" /><ref name="Yvonne et al" /> | ||
Excessive external rotation or over-rotation of the thrower’s shoulder is purportedly associated with the development of [[Internal Impingement of the Shoulder|internal impingement syndrome]] (which occurs when the [[shoulder]] is maximally externally rotated and the intra-articular side of the [[supraspinatus]] tendon impinges on the adjacent posterior superior glenoid and [[Glenoid Labrum|glenoid labrum]]). Impingement syndrome is a potential precursor to anterior shoulder instability.<ref name="Yvonne et al" /> | |||
* | |||
* | |||
Excessive external rotation or over-rotation of the thrower’s shoulder is purportedly associated with the development of internal impingement syndrome (which occurs when the shoulder is maximally externally rotated and the intra-articular side of the supraspinatus tendon impinges on the adjacent posterior superior glenoid and glenoid labrum). Impingement syndrome is a potential precursor to anterior instability.<ref name="Yvonne et al" /> | |||
{| width="100%" cellspacing="1" cellpadding="1" border="0" align="center" | {| width="100%" cellspacing="1" cellpadding="1" border="0" align="center" | ||
| Line 52: | Line 50: | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Signs and symptoms for anterior shoulder instability: | Signs and symptoms for anterior shoulder instability: | ||
* | *95% of acute traumatic dislocations.<ref name="E et al">Pope EJ, Ward JP, Rokito AS. [http://presentationgrafix.com/_dev/cake/files/archive/pdfs/241.pdf Anterior shoulder instability - a history of arthroscopic treatment.] Bull NYU Hosp Jt Dis 2011;69(1):44-9.</ref> | ||
*Dead | *[[Dead Arm Syndrome|Dead Arm syndrome]] indicates pathologic anterior instability. It occurs when the arm is in an abducted and externally rotated position. The patient complains of a sharp anterior shoulder pain and tingling in the hand and drops the arm suddenly. This syndrome is often seen in overhead sports, such as volleyball, tennis, swimming and water polo.<ref name="Yvonne et al">Satterwhite YE. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1323389/pdf/jathtrain00003-0043.pdf Evaluation and management of recurrent anterior shoulder instability.] Journal of athletic training 2000 Jul;35(3):273.</ref> | ||
*Rotator cuff weakness, particularly in external rotation and “empty-can” abduction, is common in athletes with anterior instability.<ref name="Yvonne et al" /> | *[[Rotator Cuff|Rotator cuff]] weakness, particularly in external rotation and “empty-can” abduction, is common in athletes with anterior instability.<ref name="Yvonne et al" /> | ||
*[[Bankart lesion|Bankart lesions]] are the most common consequence of traumatic anterior shoulder instability.<ref name="E et al" /> | *[[Bankart lesion|Bankart lesions]] are the most common consequence of traumatic anterior shoulder instability.<ref name="E et al" /> | ||
*Humeral avulsion of the glenohumeral ligaments is also a cause of anterior shoulder instability | *Humeral avulsion of the glenohumeral ligaments is also a cause of anterior shoulder instability.<ref name="E et al" /> | ||
*During an anterior dislocation, the posterolateral aspect of the humeral head contacts the anteroinferior rim of the glenoid, often resulting in a [[Hill Sachs Lesion|Hill | *During an anterior [[Shoulder Dislocation|dislocation]], the posterolateral aspect of the humeral head contacts the anteroinferior rim of the glenoid, often resulting in a [[Hill Sachs Lesion|Hill Sachs]] defect. This defect has been observed in up to 80% of patients with initial anterior dislocation and in 100% of patients with recurrent anterior instability.<ref name="Andrew et al" /><ref name="E et al" /> If this bony concavity engages the anterior glenoid with the arm in 90° and external rotation it is term an “Engaging Hill Sachs Lesion”, and confers a higher risk of failure following an arthroscopic stabilisation procedure<br> | ||
<br> | |||
{| width="100%" cellspacing="1" cellpadding="1" border="0" align="center" | {| width="100%" cellspacing="1" cellpadding="1" border="0" align="center" | ||
|- | |- | ||
| Line 68: | Line 63: | ||
|} | |} | ||
Symptoms related to recurrent anterior instability:<ref name="Yvonne et al" /> | |||
*Glenohumeral joint pain | *Glenohumeral joint pain | ||
*Shoulder stiffness with difficulty warming up for the | *Shoulder stiffness with difficulty warming up for the activity | ||
*Rotator cuff weakness | *[[Rotator Cuff|Rotator cuff]] weakness | ||
*Sensation of popping, grinding or catching deep in the shoulder joint | *Sensation of popping, grinding or catching deep in the [[Shoulder|shoulder joint]] | ||
*Pain when reaching backward or above shoulder height | *Pain when reaching backward or above shoulder height | ||
*Apprehension when sleeping with the arm overhead in abduction and external rotation | *Apprehension when sleeping with the arm overhead in abduction and external rotation | ||
*Neurological: | *Neurological: Tingling or burning in the lower arm and hand or localised numbness of the skin overlying the [[Deltoid|deltoid muscle]] | ||
*Tenderness of the anterior glenohumeral joint line and the posterior rotator cuff | *Tenderness of the anterior glenohumeral joint line and the posterior [[Rotator Cuff|rotator cuff]] | ||
== Differential Diagnosis== | == Differential Diagnosis== | ||
* [http://www.physio-pedia.com/Posterior_Shoulder_Instability Posterior instability] | |||
* [http://www.physio-pedia.com/Adhesive_Capsulitis Frozen shoulder/adhesive capsulitis] | |||
* [http://www.physio-pedia.com/Dead_arm_syndrome Dead arm syndrome] | |||
* [https://www.physio-pedia.com/Rotator_Cuff_Tears Rotator cuff tear] | |||
* [http://www.physio-pedia.com/index.php?title=Subacromial_Impingement Subacromial impingement] | |||
* [http://www.physio-pedia.com/index.php?title=Internal_Impingement_of_the_Shoulder Internal impingement] | |||
* [http://www.physio-pedia.com/index.php?title=Biceps_Tendonitis Biceps tendinopathy] | |||
== Diagnostic Procedure== | |||
Diagnosis of anterior shoulder instability is through a thorough history, [[X-Rays|radiology]] and three specific tests carried out in this order: [[Apprehension Test|apprehension]], [[Jobes Relocation Test|relocation]] and surprise (release) test. These tests are highly specific and strongly predictive of traumatic anterior glenohumeral instability. A fourth test, the bony apprehension test, is similar to the apprehension test, but is used to diagnose instability with a significant osseous lesion component.<ref name="Lo et al." /> | |||
== | === History<ref name="Guillaume et al." /> === | ||
GHJ instability can be categorised by the direction of instability, the chronicity, and the etiology. A thorough history and physical examination are essential. Age, activity level, sports participation, and hand dominance should be noted, as well instability in any other joints, especially the contralateral shoulder. Where a trauma is the cause of the symptoms, information about the position of the arm and the force of the trauma is noted. If this information is unknown, finding the arm position which reproduces symptoms is useful. | |||
<br>The presence and quantity of previous [[Shoulder Subluxation|shoulder subluxations]] or [[Shoulder Dislocation|dislocations]] is also important to note. Information regarding all treatment prior to presentation should be ascertained, including any period of immobilisation or physiotherapy and previous surgical interventions. The characteristics of associated pain should be noted, however, the location of pain is not a specific indicator of [[Shoulder Instability|glenohumeral instability]]. A distinction should be made between episodes of [[Shoulder Subluxation|subluxation]], or partial separation of the humeral head from the glenoid, and [[Shoulder Dislocation|dislocation]]. Any associated symptoms including neurologic deficits and functional limitations should also be assessed . Age of the patient at the first dislocation is a key prognostic indicator. Patients under 20 years with shoulder dislocations have a 90% chance of recurrence, whilst patients older than 40 years only have a 10% recurrence rate, but are more prone to [[Rotator Cuff|rotator cuff]] injuries. Patients who compete at a high level and/or in contact sports also have an increased risk of recurrence if the shoulder is treated conservatively. | |||
== | === Radiology<ref name="Guillaume et al.">Dumont GD, Russell RD, Robertson WJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3261242/ Anterior shoulder instability: a review of pathoanatomy, diagnosis and treatment.] Current reviews in musculoskeletal medicine 2011;4(4):200.</ref> === | ||
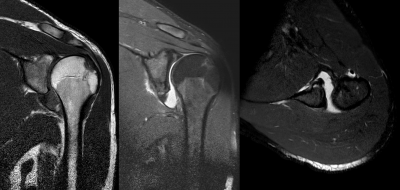
Initial [[X-Rays|images]] taken are normally anteroposterior (AP) and axillary lateral views. If pain restricts the patient's ability to tolerate an axillary lateral view, a Velpeau view may be obtained in a semi-reclined, seated position. Further views that may be useful include: AP views with the shoulder internally rotated, a West Point view, a Didiee view, and a Stryker notch view. | |||
[[Hill Sachs Lesion|Hill Sachs lesions]] are best viewed on AP radiographs in internal rotation and using a Stryker notch view. The Stryker notch view is obtained with the patient in the supine position and the arm forward flexed to 100° with the x-ray centred over the coracoid . An apical oblique view taken with the patient seated and rotated 45° and the beam directed 45° caudally is also useful for evaluating posterior humeral head defects.<ref name="Pavlov et al.">Pavlov H, Warren RF, Weiss Jr CB, Dines DM. [https://journals.lww.com/clinorthop/Abstract/1985/04000/The_Roentgenographic_Evaluation_of_Anterior.20.aspx The roentgenographic evaluation of anterior shoulder instability.] Clinical Orthopaedics and Related Research 1985;194:153-8.</ref> | |||
In cases of [[Bankart lesion|bony Bankart lesions]], recurrent [[Shoulder Instability|instability]] can cause erosive or attritional loss of the glenoid rim causing progressive instability. Loss of 20% of the glenoid rim has been shown to cause significant recurrent instability and usually requires surgical correction of the bony deficiency. This deficiency may be seen on the axillary view and may be suggested by a break in the sclerotic line encircling the glenoid rim on the AP view of the shoulder. If further investigation is needed Didiee and West Point views can be considered. The Didiee view is obtained with the patient prone and the hand is placed on the ipsilateral iliac crest with the x-ray beam directed laterally at 45° to the floor. The West Point view is obtained in a similar prone position, with the shoulder abducted to 90° and the elbow bent with the arm hanging off the table. The x-ray beam is directed 25° medially and 25° caudally. | |||
Other imaging modalities such as [[CT Scans|CT]] and [[MRI Scans|MRI]] are useful in clinical situations where the diagnosis is unclear. [[CT Scans|CT]] may be useful to demonstrate and quantify bony abnormalities including glenoid bone loss or fractures, glenoid version and humeral head abnormalities. Adding contrast and performing a CT arthrogram of the shoulder can also provide some insight into the status of the [[Glenoid Labrum|labrum]], [[Rotator Cuff|rotator cuff]] and ligamentous complex. [[MRI Scans|MRI]] is extremely useful, and the preferred method to evaluate these soft tissues, however, it does not provide as clear a picture of the associated bony injuries. In the acute setting, the hemarthrosis resulting from the dislocation serves as an intra-articular contrast medium. In the more chronic setting, gadolinium-enhanced [[MRI Scans|MRI]] is a useful modality to investigate for soft tissue pathology such as labral tears and capsular damage.<ref name="Rokous et al.">Rokous JR, Feagin JA, Abbott HG. [https://journals.lww.com/clinorthop/Citation/1972/01000/Modified_Axillary_Roentgenogram_A_Useful_Adjunct.12.aspx Modified axillary roentgenogram a useful adjunct in the diagnosis of recurrent instability of the shoulder.] Clinical Orthopaedics and Related Research 1972;82:84-6.</ref> | |||
In addition to [[Bankart lesion|Bankart lesions]], an anterior periostial sleeve avulsion (ALPSA) or a humeral avulsion of glenohumeral ligament (HAGL) can occur with an anterior shoulder dislocation. These are associated with higher recurrence rates and if missed they can lead to higher post-surgical failure rates. HAGL and ALPSA lesions are best seen using [[MRI Scans|MRI]] and MR arthrogram. | |||
== Outcome Measures == | == Outcome Measures == | ||
* [http://www.physio-pedia.com/DASH_Outcome_Measure Disabilities of the Arm, Shoulder and Hand (DASH) | * [http://www.physio-pedia.com/DASH_Outcome_Measure Disabilities of the Arm, Shoulder and Hand (DASH)] | ||
* [http://www.physio-pedia.com/Visual_Analogue_Scale Visual Analogue Scale (VAS)] | |||
* [http://www.physio-pedia.com/Visual_Analogue_Scale Visual Analogue Scale (VAS) | |||
== Examination == | == Examination == | ||
=== Special tests === | |||
==== [http://www.physio-pedia.com/index.php?title=Load_and_Shift Load and shift test]<ref name="Sandra et al.">Shultz SJ, Houglum PA, Perrin DH. Examination of musculoskeletal injuries. Human Kinetics; 2005.</ref><ref name="Farber et al." /> ==== | |||
This test can be performed with the patient in sitting or in supine. In sitting, the patient’s arm rests on the thigh with the examiner to their side and slightly behind. One hand is used to stabilise the [[scapula]] and the other is placed on the shoulder. The thumb is positioned over the posterior humeral head and fingers over the anterior humeral head. The [[humerus]] is loaded by pushing the humeral head into a neutral position within the fossa. Whilst maintaining the humeral head in this position, [[humerus]] is shifted forwards by applying an anterior force, to asses anterior instability. Some movement is normal, but should not be more than 25% of the humeral head. | |||
Instability is classified as follows: | |||
* Grade 1: Shift between 25% and 50% | |||
* Grade 2: More than 50% shift with spontaneous reduction when the force is stopped, | |||
* Grade 3: More than 50% shift without spontaneous reduction and remains dislocated. A combination of laxity and a reproduction of the symptoms determines a positive or negative result. <br> | |||
{{#ev:youtube|rj6bQivN2h4|300}} | |||
==== [http://www.physio-pedia.com/Apprehension_Test Apprehension], [http://www.physio-pedia.com/Jobes_Relocation_Test Relocation] and anterior release tests<ref name="Farber et al.">Farber AJ, Castillo R, Clough M, Bahk M, McFarland EG. [http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.866.5638&rep=rep1&type=pdf Clinical assessment of three common tests for traumatic anterior shoulder instability.] JBJS 2006;88(7):1467-74.</ref><ref name="Savoie et al.">Savoie III FH, O’Brien MJ. [https://journals.lww.com/sportsmedarthro/Abstract/2014/06000/Anterior_Instability_in_the_Throwing_Shoulder.8.aspx Anterior instability in the throwing shoulder.] Sports Medicine and Arthroscopy Review 2014;22(2):117-9.</ref> ==== | |||
The patient is in a supine position, with the [[shoulder]] in 90° of abduction and maximal lateral rotation. A positive apprehension test occurs if the patient either looks apprehensive or resists further movement. To differentiate apprehension from other potential conditions, the relocation test is used. Start position is the same as that for the apprehension test, then an anterior-posterior force is applied to the shoulder to relocate the [[humerus]] in the fossa. The apprehension will decrease in the case of shoulder instability. The final test is the release test, where the posteriorly directed force applied in the relocation test is removed. The result is considered positive if the patient’s apprehension returns. | |||
{| border="0" cellspacing="1" cellpadding="1" | |||
|- | |||
|{{#ev:youtube|qHDXhrhltwE|300}} | |||
|{{#ev:youtube|6Yb-oiJkbnM|300}} | |||
|{{#ev:youtube|CBZq_MyTHQE|300}} | |||
|} | |||
==== Anterior drawer test<ref name="Lo et al.">Lo IK, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. [https://www.researchgate.net/profile/Michael_Woolfrey/publication/8686670_An_Evaluation_of_the_Apprehension_Relocation_and_Surprise_Tests_for_Anterior_Shoulder_Instability/links/0c96053a96e053033e000000.pdf An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability.] The American Journal of Sports Medicine 2004;32(2):301-7.</ref><ref name="Milgrom et al.">Milgrom C, Milgrom Y, Radeva-Petrova D, Jaber S, Beyth S, Finestone AS. [https://www.sciencedirect.com/science/article/abs/pii/S1058274614004248 The supine apprehension test helps predict the risk of recurrent instability after a first-time anterior shoulder dislocation.] Journal of shoulder and elbow surgery 2014;23(12):1838-42.</ref> ==== | |||
The patient is in a supine position and the affected shoulder over the edge of the table. The patient’s arm should be relaxed. Position the arm in a combined midrange abducted position with forward flexion and lateral rotation. The stabilising hand is placed on the scapula so that the fingers and thumb secure the [[scapula]] at the spine of the scapula and the coracoid. The patient’s arm is pulled anteriorly to apply a gliding force to the glenohumeral joint. If an audible click is heard during the movement, the [[Glenoid Labrum|glenoid labrum]] may be torn, or the joint may be sufficiently lax to allow the humeral head to glide over the glenoid labrum rim. | |||
{{#ev:youtube|G8s_7Q5zfTM|300}} | |||
== Medical Management == | == Medical Management == | ||
Analgesics can be used to decrease pain<ref name="mph">Wilson SR, Price DD. Shoulder Dislocation in Emergency Medicine. Medscape; 2011.</ref> with the patient in a position of comfort while maintaining cervical spine immobilisation where necessary. A pillow is placed between the patient's arm and torso to further increase comfort. | |||
== Physiotherapy Management == | |||
A conservative rehabilitation program needs to be patient specific, based on the type and degree of [[Shoulder Instability|shoulder instability]] present and the desired level of return to function. A rehabilitation programme can consist of a combination of any of the following: Strengthening exercises, dynamic stabilisation drills, neuromuscular training, proprioception drills, scapular muscle strengthening and a graded return to the desired activities. <br> | |||
=== Rehabilitation factors === | |||
Seven key factors should be considered when designing a rehabilitation program: | |||
* <u>Onset of pathology</u>: Pathological [[Shoulder Instability|shoulder instability]] may result from an acute, traumatic event or chronic, recurrent instability. The goal of the rehabilitation program may vary greatly based on the onset and mechanism of injury. Following a traumatic [[Shoulder Subluxation|subluxation]] or [[Shoulder Dislocation|dislocation]], the patient typically presents with significant soft tissue trauma, pain, and apprehension. Rehabilitation for the patient with a first-time traumatic episode will be progressed based on the patient's symptoms with emphasis on early controlled range of motion, reduction of muscle spasms and guarding, and relief of pain.<br>Conversely, a patient presenting with atraumatic instability often presents with a history of repetitive injuries and symptomatic complaints. Rehabilitation for this patient should focus on early proprioception training, dynamic stabilization drills, neuromuscular control, scapular muscle exercises, and muscle strengthening exercises to enhance dynamic stability due to the unique characteristic of excessive capsular laxity and capsular redundancy in this type of patient. | |||
* <u>Degree of instability</u>: The second factor is the degree of instability present in the patient and the effect on their function. <br>The rate of progression of the rehabilitation program will vary based upon the degree of instability and persistence of symptoms. For example, a patient with mild [[Shoulder Subluxation|subluxations]] and muscle guarding may initially tolerate strengthening exercises and neuromuscular control drills more than a patient with a significant amount of muscular guarding. | |||
* <u>Frequency of [[Shoulder Dislocation|dislocation]]:</u> The primary traumatic [[Shoulder Dislocation|dislocation]] is most often treated conservatively with immobilisation in a sling and early, controlled passive range of motion exercises, especially with first time [[Shoulder Dislocation|dislocations]]. Chronic subluxations, as seen in the atraumatic, unstable shoulder may be treated more aggressively due to the lack of acute tissue damage and less muscular guarding and inflammation. Rotator cuff and periscapular strengthening activities should be initiated while ROM exercises are progressed. Caution is placed on avoiding excessive stretching of the joint capsule through aggressive ROM activities. The goal is to enhance strength, proprioception, dynamic stability and neuromuscular control, especially in the specific points of motion or direction which results in instability complaints. | |||
* <u>Direction of [[Shoulder Instability|instability]]:</u> Anterior [[Shoulder Instability|instability]] is the most common traumatic type of instability seen clinically, where the humeral head is forced into extremes of abduction and external rotation, or horizontal abduction, the glenolabral complex and capsule may become detached from the glenoid rim. | |||
* <u>Concomitant pathologies:</u> Other soft tissue need to be considered that may have been affected as well as the pre-morbid status of the soft tissue. These concomitant lesions may significantly slow down the rehabilitation program in order to protect the healing tissue. | |||
* <u>Neuromuscular control:</u> The sixth factor to consider is the patient's level of neuromuscular control, particularly at end range of motion. | |||
* <u>Activity level:</u> The final factor to consider in the conservative rehabilitation of the unstable [[shoulder]] is arm dominance and the desired activity level of the patient. If the patient frequently performs an overhead motion or sporting activities such as a tennis, volleyball, or a throwing sport, then the rehabilitation program should include sport specific dynamic stabilisation exercises, neuromuscular control drills, and plyometric exercises in the overhead position once full, pain free ROM and adequate strength has been achieved. Patients whose functional demands involve below [[shoulder]] level activities will follow a progressive exercise program to return to full ROM and strength.<br> | |||
=== Rehabilitation guidelines === | |||
Patients may be classified into two common forms of shoulder instability, traumatic and atraumatic. There are specific guidelines to consider in individualising the rehabilitation of each patient. | |||
==== Traumatic Shoulder Instability<ref name="Kevin et al.">Wilk KE, Macrina LC, Reinold MM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2953282/ Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability.] North American journal of sports physical therapy 2006;1(1):16.</ref><ref name="Burkhead et al.">Burkhead Jr WZ, Rockwood Jr CA. [https://www.orthopedicsports.com/wp-content/themes/ypo-theme/pdf/treatment-instability-shoulder-exercise-program.pdf Treatment of instability of the shoulder with an exercise program.] JBJS 1992;74(6):890-6.</ref> ==== | |||
===== The program will vary in length for each individual depending on the seven rehabilitation factors. ===== | |||
===== Phase I: Acute motion phase ===== | |||
Goals: | |||
* Protect healing capsular structures | |||
* Re-establish pain-free range of motion | |||
* Decrease pain, inflammation, and muscular spasms | |||
* Retard muscular atrophy/establish voluntary muscle activity | |||
* Re-establish dynamic stability | |||
* Improve proprioception | |||
<br>Exercises: | |||
* Range of motion: Pendulums, rope and pulley, active-assisted ROM (F, IR, ER) | |||
* Strengthening/proprioception: Isometrics (flexion, abduction, extension, IR, ER, performed with arm at side) | |||
* Rhythmic stabilisation: ER/IR/F/E in scapular plane, weight shifts (standing hands on table), proprioception training drills (active joint reproduction: F/ IR/ER) | |||
During the early rehabilitation program, caution must be applied in placing the capsule under stress until dynamic joint stability is restored. It is important to refrain from pushing into external rotation or horizontal abduction with anterior instability. | |||
== | ===== Phase II: Intermediate phase ===== | ||
Criteria to Progress to Phase II: | |||
* Nearly full to full passive ROM (ER may still be limited) | |||
* Minimal pain or tenderness | |||
* Good MMT of IR, ER, flexion and abduction | |||
* Baseline proprioception and dynamic stability | |||
Goals: | |||
* Regain and improve muscular strength | |||
* Normalise arthrokinematics | |||
* Enhance proprioception and kinesthesia | |||
* Enhance dynamic stabilisation | |||
* Improve neuromuscular control of [[Shoulder|shoulder complex]] | |||
<br>Exercises: | |||
* Progress ROM activities at 90° abduction to tolerance (pain free) | |||
* Initiate isotonic strengthening | |||
* Emphasis ER and scapular strengthening: Abduction to 90°, side lying ER to 45°, push-ups onto table, biceps curls, triceps pushdowns, prone rowing | |||
* Improve neuromuscular control of shoulder complex: PNF, wall stabilisation using a ball, static holds in push-up position on ball. | |||
===== Phase III: Advanced strengthening phase ===== | |||
Criteria to Progress to Phase III: | |||
* Full non-painful range of motion | |||
* No palpable tenderness | |||
* Continued progression of resistive exercises | |||
* Normal muscle strength, dynamic stability and neuromuscular control | |||
Goals: | |||
* Improve strength/power/endurance | |||
* Improve neuromuscular control | |||
* Enhance dynamic stabilisations | |||
* Prepare patient/athlete for activity | |||
<br>Exercises: | |||
* Continue isotonic strengthening (progress resistance): Full ROM strengthening, bench press in restricted ROM, flat and incline chest press | |||
* Emphasise PNF | |||
* Advanced neuromuscular control drills: Ball flips on table, push-ups on ball with rhythmic stabilisations, manual scapular neuromuscular control drills, initiate perturbation activities | |||
* Endurance training: Timed bouts of exercises (30-60s), increase number of repetitions, multiple bouts throughout day | |||
* Initiate plyometric training: 2 hand-drills (chest pass throw, side to side throw, overhead soccer throw) and progress to 1 hand-drills (wall dribbles, 90/90 baseball throws) | |||
===== Phase IV: Return to activity phase ===== | |||
Criteria to Progress to Phase IV: | |||
* Full ROM | |||
* No pain or palpable tenderness | |||
* Satisfactory isokinetic test | |||
* Satisfactory clinical exam | |||
Goals: | |||
* Maintain optimal level of strength/power/endurance | |||
* Progressively increase activity level to prepare patient/athlete for full functional return to activity/sport | |||
<br>Exercises: | |||
* Continue all exercises as in phase III | |||
* Progress isotonic strengthening exercises | |||
* Resume normal lifting program | |||
* Initiate interval sport program | |||
===== Follow up ===== | |||
* Isokinetic test (ER/IR/Abd/Add) | |||
* Progress interval program | |||
* Maintenance of exercise program | |||
==== Atraumatic Instability<ref name="Kevin et al." /><ref name="Burkhead et al." /> ==== | |||
This multi-phased program is designed to allow the patient/athlete to return to their previous functional level as quickly and safely as possible. Each phase will vary in length for each individual depending upon the severity of injury, ROM and strength deficits, and the required activity demands of the patient. | |||
===== Phase I: Acute phase ===== | |||
Goals: | |||
* Decrease pain/inflammation | |||
* Re-establish functional range of motion | |||
* Establish voluntary muscular activation | |||
* Re-establish muscular balance | |||
* Improve proprioception | |||
* Decrease pain and inflammation | |||
* Therapeutic modalities (i.e. [[Cryotherapy|ice]], electrotherapy) | |||
* NSAIDs | |||
* Gentle joint mobilisations (Grade I and II) for neuromodulation of pain | |||
Exercises: | |||
* Refrain from activities and motion in extremes of ROM | |||
* ROM exercises: Pendulum, rope and pulley | |||
* Strengthening exercises: Isometric, flexion, abduction, extension | |||
* Proprioception | |||
* Active joint reposition drills for ER/IR | |||
===== Phase II: Intermediate phase ===== | |||
Criteria to Progress to Phase II: | |||
* Full functional ROM | |||
* Minimal pain or tenderness | |||
* “Good” MMT | |||
Goals: | |||
* Normalise arthrokinematics of [[Shoulder|shoulder complex]] | |||
* Regain and improve muscular strength of glenohumeral and scapular muscles | |||
* Improve neuromuscular control of shoulder complex | |||
* Enhance proprioception and kinesthesia | |||
Exercises: | |||
* Initiate isotonic strengthening: IR/ER (sideling dumbbell), abduction to 90° | |||
* Initiate eccentric exercises at 0° abduction, IR/ER | |||
* Improve neuromuscular control of shoulder complex: Rhythmic stabilisation drills at inner, mid, and outer ROM, proprioceptive, scapulothoracic/glenohumeral musculature, PNF, weight shifts hand on ball, wall stabilisation drills. | |||
== | ===== Phase III: Advanced strengthening phase ===== | ||
Criteria to Progress to Phase III: | |||
* Full pain-free ROM | |||
* No pain or tenderness | |||
* Continued progression of resistive exercises | |||
* Good to normal muscle strength | |||
Goals: | |||
* Enhance dynamic stabilisation | |||
* Improve strength/endurance | |||
* Improve neuromuscular control | |||
* Prepare patient for activity | |||
Exercises: | |||
* Continue isotonic strengthening | |||
* Continue eccentric strengthening | |||
* Emphasise PNF exercises with rhythmic stabilisation hold | |||
* Continue to progress neuromuscular control drills: push-ups with rhythmic stabilisation, progress to unsteady surface, medicine ball, rocker board | |||
* Program scapular neuromuscular control training: Sidelyng manual drills | |||
* Emphasise endurance training: Timed sessions of exercise (30-60s), increasing number of reps | |||
===== Phase IV - Return to activity phase ===== | |||
Goals: | |||
* Maintain optimal level of strength/power/endurance | |||
* Progressively increase activity level to prepare patient/athlete for full functional return to activity/sport | |||
Exercises: | |||
* Continue all exercises as in phase III | |||
* Initiate interval sport program | |||
* Patient education | |||
Criteria to Progress to Phase IV: | |||
* Full ROM | |||
* No pain or palpable tenderness | |||
* Satisfactory isokinetic test | |||
* Satisfactory clinical exam | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
* [[Shoulder Instability|Shoulder instability]] may have a traumatic or atraumatic cause. | |||
* Anterior shoulder instability is an injury to the [[Shoulder|shoulder joint]] so that the upper arm is displaced from its normal position in glenoid and the joint surfaces no longer contact each other. | |||
* Anterior [[Shoulder Dislocation|shoulder dislocations]] are much more common than posterior dislocations. | |||
* The recurrence rate after primary [[Shoulder Dislocation|shoulder dislocation]] is greatest in individuals less than 20 years old. Anterior instability accounts for 95% of acute traumatic dislocations. | |||
* Diagnosis of anterior shoulder instability is made through history, [[X-Rays|radiology]] and the following three tests: [[Apprehension Test|apprehension]], [[Jobes Relocation Test|relocation]] and surprise (release) test, performed respectively. | |||
* Rehabilitation should be based on an individual basis with consideration to the patient’s pre-morbid state and level of activity. | |||
== References: == | |||
== References == | |||
<references /> | <references /> | ||
[[Category:Vrije_Universiteit_Brussel_Project]] [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] [[Category:Shoulder]] [[Category: | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Shoulder]] | |||
[[Category:Conditions]] | |||
[[Category:Shoulder - Conditions]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
Latest revision as of 10:50, 9 January 2023
Top Contributors - Laura Ritchie, Scott Cornish, Andeela Hafeez, Admin, Leana Louw, Kim Jackson, Liesbeth De Feyter, Fasuba Ayobami, 127.0.0.1, Tony Lowe, Wanda van Niekerk, Borms Killian, Naomi O'Reilly and Kai A. Sigel
Definition[edit | edit source]
The term anterior shoulder instability refers to a shoulder in which soft tissue or bony insult allows the humeral head to sublux or dislocate from the glenoid fossa.[1] It is an injury to the glenohumeral joint (GHJ) where the humerus is displaced from its normal position in the center of the glenoid fossa and the joint surfaces no longer touch each other.
Also see related pages for shoulder instability, Shoulder Subluxation and shoulder dislocation.
Clinically Relevant Anatomy[edit | edit source]
The glenohumeral joint (multi-axial spheroidal joint) is one of the largest and most complex joints in the body. It has the greatest range of movement of any joint, but this leaves it inherently unstable and with the highest chance of dislocation of all the body's joints. The GHJ is formed where the humeral head fits into the glenoid fossa, an irregular oval shape, which is an extension of the scapula, like a ball and socket, although only 25% of the humeral head makes contact with the glenoid fossa at any time.
This joint is surrounded by numerous ligaments and muscles which give it stability. The surrounding capsule may also add some stability with the coracohumeral and glenohumeral ligaments reinforcing the capsule. Other important bones in the shoulder include:
- The acromion: a bony projection off the scapula
- The clavicle: which joins the acromion via the acromioclavicular joint and distal sternoclavicular joint to the axial skeleton
- The coracoid process: a hook-like bony projection from the scapula
The shoulder has several other important structures:
- The rotator cuff: A collection of 4 muscles originating from the scapula (supraspinatus, infraspinatus, subscapularis and teres minor) which stabilise the GHJ and allow the wide range of motion.
- The bursae: There are a number of bursae associated with the shoulder of which the subacromial bursa is the one most likely to become symptomatic with bursitis. It sits between the superior surface of the supraspinatus tendon and the acromium, coracoid an the coracoacromial ligament, extending down over the humeral tendinous attachment of supraspinatus
- The labrum: A fibrous ring of cartilage which extends up from the glenoid providing stability in the form of a deeper cup for the humeral head to fit into.[2]
Epidemiology /Etiology[edit | edit source]
Epidemiology[edit | edit source]
Anterior shoulder dislocations are much more common than posterior dislocations.[3]
Research suggests that incidence of recurrent shoulder dislocation is significantly higher in younger patients.[4][5] The consequences of an initial anterior glenohumeral dislocation in patients over forty years of age are quite different than in the younger population, primarily due to the increased incidence of rotator cuff tears and associated neurovascular injuries. The anterior or posterior supporting structures of the shoulder can also be disrupted following an anterior dislocation. In the younger population, anterior capsuloligamentous structures most commonly fail, whereas in older patients with pre-existing degenerative weakening of the rotator cuff, the posterior structures are more likely to fail.[4]
Etiology[edit | edit source]
The GHJ is stabilised by both dynamic and static structures.[4]
- Dynamic stabilisers: Rotator cuff muscles, Biceps Brachii, deltoid
- Static stabilisers: Glenohumeral joint capsule, the glenohumeral ligaments, the labrum, negative pressure within the joint capsule, and the bony congruity of the joint.[3][5]
- The labrum: This concave compression mechanism plays an important role in the stability of the glenohumeral joint by maintaining the localisation of the humeral head at the glenoid against translational forces. The glenoid concavity is established by the glenoid shape, the glenoid cartilage and the glenoid labrum. The glenoid labrum increases the width and depth of the glenoid. Instability is increased with the size of the glenoid defect.[6]
- The glenohumeral ligaments: The superior glenohumeral ligament functions primarily to resist inferior translation and external rotation of the humeral head in the adducted arm. The middle glenohumeral ligament functions primarily to resist external rotation from 0° to 90° and provides anterior stability to the moderately abducted shoulder. The inferior glenohumeral ligament is composed of two bands, anterior and posterior, and the intervening capsule. The primary function of the anterior band is to resist anteroinferior translation.[5][7]
Excessive external rotation or over-rotation of the thrower’s shoulder is purportedly associated with the development of internal impingement syndrome (which occurs when the shoulder is maximally externally rotated and the intra-articular side of the supraspinatus tendon impinges on the adjacent posterior superior glenoid and glenoid labrum). Impingement syndrome is a potential precursor to anterior shoulder instability.[7]
Characteristics/Clinical Presentation[edit | edit source]
Signs and symptoms for anterior shoulder instability:
- 95% of acute traumatic dislocations.[5]
- Dead Arm syndrome indicates pathologic anterior instability. It occurs when the arm is in an abducted and externally rotated position. The patient complains of a sharp anterior shoulder pain and tingling in the hand and drops the arm suddenly. This syndrome is often seen in overhead sports, such as volleyball, tennis, swimming and water polo.[7]
- Rotator cuff weakness, particularly in external rotation and “empty-can” abduction, is common in athletes with anterior instability.[7]
- Bankart lesions are the most common consequence of traumatic anterior shoulder instability.[5]
- Humeral avulsion of the glenohumeral ligaments is also a cause of anterior shoulder instability.[5]
- During an anterior dislocation, the posterolateral aspect of the humeral head contacts the anteroinferior rim of the glenoid, often resulting in a Hill Sachs defect. This defect has been observed in up to 80% of patients with initial anterior dislocation and in 100% of patients with recurrent anterior instability.[3][5] If this bony concavity engages the anterior glenoid with the arm in 90° and external rotation it is term an “Engaging Hill Sachs Lesion”, and confers a higher risk of failure following an arthroscopic stabilisation procedure
Symptoms related to recurrent anterior instability:[7]
- Glenohumeral joint pain
- Shoulder stiffness with difficulty warming up for the activity
- Rotator cuff weakness
- Sensation of popping, grinding or catching deep in the shoulder joint
- Pain when reaching backward or above shoulder height
- Apprehension when sleeping with the arm overhead in abduction and external rotation
- Neurological: Tingling or burning in the lower arm and hand or localised numbness of the skin overlying the deltoid muscle
- Tenderness of the anterior glenohumeral joint line and the posterior rotator cuff
Differential Diagnosis[edit | edit source]
- Posterior instability
- Frozen shoulder/adhesive capsulitis
- Dead arm syndrome
- Rotator cuff tear
- Subacromial impingement
- Internal impingement
- Biceps tendinopathy
Diagnostic Procedure[edit | edit source]
Diagnosis of anterior shoulder instability is through a thorough history, radiology and three specific tests carried out in this order: apprehension, relocation and surprise (release) test. These tests are highly specific and strongly predictive of traumatic anterior glenohumeral instability. A fourth test, the bony apprehension test, is similar to the apprehension test, but is used to diagnose instability with a significant osseous lesion component.[8]
History[9][edit | edit source]
GHJ instability can be categorised by the direction of instability, the chronicity, and the etiology. A thorough history and physical examination are essential. Age, activity level, sports participation, and hand dominance should be noted, as well instability in any other joints, especially the contralateral shoulder. Where a trauma is the cause of the symptoms, information about the position of the arm and the force of the trauma is noted. If this information is unknown, finding the arm position which reproduces symptoms is useful.
The presence and quantity of previous shoulder subluxations or dislocations is also important to note. Information regarding all treatment prior to presentation should be ascertained, including any period of immobilisation or physiotherapy and previous surgical interventions. The characteristics of associated pain should be noted, however, the location of pain is not a specific indicator of glenohumeral instability. A distinction should be made between episodes of subluxation, or partial separation of the humeral head from the glenoid, and dislocation. Any associated symptoms including neurologic deficits and functional limitations should also be assessed . Age of the patient at the first dislocation is a key prognostic indicator. Patients under 20 years with shoulder dislocations have a 90% chance of recurrence, whilst patients older than 40 years only have a 10% recurrence rate, but are more prone to rotator cuff injuries. Patients who compete at a high level and/or in contact sports also have an increased risk of recurrence if the shoulder is treated conservatively.
Radiology[9][edit | edit source]
Initial images taken are normally anteroposterior (AP) and axillary lateral views. If pain restricts the patient's ability to tolerate an axillary lateral view, a Velpeau view may be obtained in a semi-reclined, seated position. Further views that may be useful include: AP views with the shoulder internally rotated, a West Point view, a Didiee view, and a Stryker notch view.
Hill Sachs lesions are best viewed on AP radiographs in internal rotation and using a Stryker notch view. The Stryker notch view is obtained with the patient in the supine position and the arm forward flexed to 100° with the x-ray centred over the coracoid . An apical oblique view taken with the patient seated and rotated 45° and the beam directed 45° caudally is also useful for evaluating posterior humeral head defects.[10]
In cases of bony Bankart lesions, recurrent instability can cause erosive or attritional loss of the glenoid rim causing progressive instability. Loss of 20% of the glenoid rim has been shown to cause significant recurrent instability and usually requires surgical correction of the bony deficiency. This deficiency may be seen on the axillary view and may be suggested by a break in the sclerotic line encircling the glenoid rim on the AP view of the shoulder. If further investigation is needed Didiee and West Point views can be considered. The Didiee view is obtained with the patient prone and the hand is placed on the ipsilateral iliac crest with the x-ray beam directed laterally at 45° to the floor. The West Point view is obtained in a similar prone position, with the shoulder abducted to 90° and the elbow bent with the arm hanging off the table. The x-ray beam is directed 25° medially and 25° caudally.
Other imaging modalities such as CT and MRI are useful in clinical situations where the diagnosis is unclear. CT may be useful to demonstrate and quantify bony abnormalities including glenoid bone loss or fractures, glenoid version and humeral head abnormalities. Adding contrast and performing a CT arthrogram of the shoulder can also provide some insight into the status of the labrum, rotator cuff and ligamentous complex. MRI is extremely useful, and the preferred method to evaluate these soft tissues, however, it does not provide as clear a picture of the associated bony injuries. In the acute setting, the hemarthrosis resulting from the dislocation serves as an intra-articular contrast medium. In the more chronic setting, gadolinium-enhanced MRI is a useful modality to investigate for soft tissue pathology such as labral tears and capsular damage.[11]
In addition to Bankart lesions, an anterior periostial sleeve avulsion (ALPSA) or a humeral avulsion of glenohumeral ligament (HAGL) can occur with an anterior shoulder dislocation. These are associated with higher recurrence rates and if missed they can lead to higher post-surgical failure rates. HAGL and ALPSA lesions are best seen using MRI and MR arthrogram.
Outcome Measures[edit | edit source]
Examination[edit | edit source]
Special tests[edit | edit source]
Load and shift test[12][13][edit | edit source]
This test can be performed with the patient in sitting or in supine. In sitting, the patient’s arm rests on the thigh with the examiner to their side and slightly behind. One hand is used to stabilise the scapula and the other is placed on the shoulder. The thumb is positioned over the posterior humeral head and fingers over the anterior humeral head. The humerus is loaded by pushing the humeral head into a neutral position within the fossa. Whilst maintaining the humeral head in this position, humerus is shifted forwards by applying an anterior force, to asses anterior instability. Some movement is normal, but should not be more than 25% of the humeral head.
Instability is classified as follows:
- Grade 1: Shift between 25% and 50%
- Grade 2: More than 50% shift with spontaneous reduction when the force is stopped,
- Grade 3: More than 50% shift without spontaneous reduction and remains dislocated. A combination of laxity and a reproduction of the symptoms determines a positive or negative result.
Apprehension, Relocation and anterior release tests[13][14][edit | edit source]
The patient is in a supine position, with the shoulder in 90° of abduction and maximal lateral rotation. A positive apprehension test occurs if the patient either looks apprehensive or resists further movement. To differentiate apprehension from other potential conditions, the relocation test is used. Start position is the same as that for the apprehension test, then an anterior-posterior force is applied to the shoulder to relocate the humerus in the fossa. The apprehension will decrease in the case of shoulder instability. The final test is the release test, where the posteriorly directed force applied in the relocation test is removed. The result is considered positive if the patient’s apprehension returns.
Anterior drawer test[8][15][edit | edit source]
The patient is in a supine position and the affected shoulder over the edge of the table. The patient’s arm should be relaxed. Position the arm in a combined midrange abducted position with forward flexion and lateral rotation. The stabilising hand is placed on the scapula so that the fingers and thumb secure the scapula at the spine of the scapula and the coracoid. The patient’s arm is pulled anteriorly to apply a gliding force to the glenohumeral joint. If an audible click is heard during the movement, the glenoid labrum may be torn, or the joint may be sufficiently lax to allow the humeral head to glide over the glenoid labrum rim.
Medical Management[edit | edit source]
Analgesics can be used to decrease pain[16] with the patient in a position of comfort while maintaining cervical spine immobilisation where necessary. A pillow is placed between the patient's arm and torso to further increase comfort.
Physiotherapy Management[edit | edit source]
A conservative rehabilitation program needs to be patient specific, based on the type and degree of shoulder instability present and the desired level of return to function. A rehabilitation programme can consist of a combination of any of the following: Strengthening exercises, dynamic stabilisation drills, neuromuscular training, proprioception drills, scapular muscle strengthening and a graded return to the desired activities.
Rehabilitation factors[edit | edit source]
Seven key factors should be considered when designing a rehabilitation program:
- Onset of pathology: Pathological shoulder instability may result from an acute, traumatic event or chronic, recurrent instability. The goal of the rehabilitation program may vary greatly based on the onset and mechanism of injury. Following a traumatic subluxation or dislocation, the patient typically presents with significant soft tissue trauma, pain, and apprehension. Rehabilitation for the patient with a first-time traumatic episode will be progressed based on the patient's symptoms with emphasis on early controlled range of motion, reduction of muscle spasms and guarding, and relief of pain.
Conversely, a patient presenting with atraumatic instability often presents with a history of repetitive injuries and symptomatic complaints. Rehabilitation for this patient should focus on early proprioception training, dynamic stabilization drills, neuromuscular control, scapular muscle exercises, and muscle strengthening exercises to enhance dynamic stability due to the unique characteristic of excessive capsular laxity and capsular redundancy in this type of patient. - Degree of instability: The second factor is the degree of instability present in the patient and the effect on their function.
The rate of progression of the rehabilitation program will vary based upon the degree of instability and persistence of symptoms. For example, a patient with mild subluxations and muscle guarding may initially tolerate strengthening exercises and neuromuscular control drills more than a patient with a significant amount of muscular guarding. - Frequency of dislocation: The primary traumatic dislocation is most often treated conservatively with immobilisation in a sling and early, controlled passive range of motion exercises, especially with first time dislocations. Chronic subluxations, as seen in the atraumatic, unstable shoulder may be treated more aggressively due to the lack of acute tissue damage and less muscular guarding and inflammation. Rotator cuff and periscapular strengthening activities should be initiated while ROM exercises are progressed. Caution is placed on avoiding excessive stretching of the joint capsule through aggressive ROM activities. The goal is to enhance strength, proprioception, dynamic stability and neuromuscular control, especially in the specific points of motion or direction which results in instability complaints.
- Direction of instability: Anterior instability is the most common traumatic type of instability seen clinically, where the humeral head is forced into extremes of abduction and external rotation, or horizontal abduction, the glenolabral complex and capsule may become detached from the glenoid rim.
- Concomitant pathologies: Other soft tissue need to be considered that may have been affected as well as the pre-morbid status of the soft tissue. These concomitant lesions may significantly slow down the rehabilitation program in order to protect the healing tissue.
- Neuromuscular control: The sixth factor to consider is the patient's level of neuromuscular control, particularly at end range of motion.
- Activity level: The final factor to consider in the conservative rehabilitation of the unstable shoulder is arm dominance and the desired activity level of the patient. If the patient frequently performs an overhead motion or sporting activities such as a tennis, volleyball, or a throwing sport, then the rehabilitation program should include sport specific dynamic stabilisation exercises, neuromuscular control drills, and plyometric exercises in the overhead position once full, pain free ROM and adequate strength has been achieved. Patients whose functional demands involve below shoulder level activities will follow a progressive exercise program to return to full ROM and strength.
Rehabilitation guidelines[edit | edit source]
Patients may be classified into two common forms of shoulder instability, traumatic and atraumatic. There are specific guidelines to consider in individualising the rehabilitation of each patient.
Traumatic Shoulder Instability[17][18][edit | edit source]
The program will vary in length for each individual depending on the seven rehabilitation factors.[edit | edit source]
Phase I: Acute motion phase[edit | edit source]
Goals:
- Protect healing capsular structures
- Re-establish pain-free range of motion
- Decrease pain, inflammation, and muscular spasms
- Retard muscular atrophy/establish voluntary muscle activity
- Re-establish dynamic stability
- Improve proprioception
Exercises:
- Range of motion: Pendulums, rope and pulley, active-assisted ROM (F, IR, ER)
- Strengthening/proprioception: Isometrics (flexion, abduction, extension, IR, ER, performed with arm at side)
- Rhythmic stabilisation: ER/IR/F/E in scapular plane, weight shifts (standing hands on table), proprioception training drills (active joint reproduction: F/ IR/ER)
During the early rehabilitation program, caution must be applied in placing the capsule under stress until dynamic joint stability is restored. It is important to refrain from pushing into external rotation or horizontal abduction with anterior instability.
Phase II: Intermediate phase[edit | edit source]
Criteria to Progress to Phase II:
- Nearly full to full passive ROM (ER may still be limited)
- Minimal pain or tenderness
- Good MMT of IR, ER, flexion and abduction
- Baseline proprioception and dynamic stability
Goals:
- Regain and improve muscular strength
- Normalise arthrokinematics
- Enhance proprioception and kinesthesia
- Enhance dynamic stabilisation
- Improve neuromuscular control of shoulder complex
Exercises:
- Progress ROM activities at 90° abduction to tolerance (pain free)
- Initiate isotonic strengthening
- Emphasis ER and scapular strengthening: Abduction to 90°, side lying ER to 45°, push-ups onto table, biceps curls, triceps pushdowns, prone rowing
- Improve neuromuscular control of shoulder complex: PNF, wall stabilisation using a ball, static holds in push-up position on ball.
Phase III: Advanced strengthening phase[edit | edit source]
Criteria to Progress to Phase III:
- Full non-painful range of motion
- No palpable tenderness
- Continued progression of resistive exercises
- Normal muscle strength, dynamic stability and neuromuscular control
Goals:
- Improve strength/power/endurance
- Improve neuromuscular control
- Enhance dynamic stabilisations
- Prepare patient/athlete for activity
Exercises:
- Continue isotonic strengthening (progress resistance): Full ROM strengthening, bench press in restricted ROM, flat and incline chest press
- Emphasise PNF
- Advanced neuromuscular control drills: Ball flips on table, push-ups on ball with rhythmic stabilisations, manual scapular neuromuscular control drills, initiate perturbation activities
- Endurance training: Timed bouts of exercises (30-60s), increase number of repetitions, multiple bouts throughout day
- Initiate plyometric training: 2 hand-drills (chest pass throw, side to side throw, overhead soccer throw) and progress to 1 hand-drills (wall dribbles, 90/90 baseball throws)
Phase IV: Return to activity phase[edit | edit source]
Criteria to Progress to Phase IV:
- Full ROM
- No pain or palpable tenderness
- Satisfactory isokinetic test
- Satisfactory clinical exam
Goals:
- Maintain optimal level of strength/power/endurance
- Progressively increase activity level to prepare patient/athlete for full functional return to activity/sport
Exercises:
- Continue all exercises as in phase III
- Progress isotonic strengthening exercises
- Resume normal lifting program
- Initiate interval sport program
Follow up[edit | edit source]
- Isokinetic test (ER/IR/Abd/Add)
- Progress interval program
- Maintenance of exercise program
Atraumatic Instability[17][18][edit | edit source]
This multi-phased program is designed to allow the patient/athlete to return to their previous functional level as quickly and safely as possible. Each phase will vary in length for each individual depending upon the severity of injury, ROM and strength deficits, and the required activity demands of the patient.
Phase I: Acute phase[edit | edit source]
Goals:
- Decrease pain/inflammation
- Re-establish functional range of motion
- Establish voluntary muscular activation
- Re-establish muscular balance
- Improve proprioception
- Decrease pain and inflammation
- Therapeutic modalities (i.e. ice, electrotherapy)
- NSAIDs
- Gentle joint mobilisations (Grade I and II) for neuromodulation of pain
Exercises:
- Refrain from activities and motion in extremes of ROM
- ROM exercises: Pendulum, rope and pulley
- Strengthening exercises: Isometric, flexion, abduction, extension
- Proprioception
- Active joint reposition drills for ER/IR
Phase II: Intermediate phase[edit | edit source]
Criteria to Progress to Phase II:
- Full functional ROM
- Minimal pain or tenderness
- “Good” MMT
Goals:
- Normalise arthrokinematics of shoulder complex
- Regain and improve muscular strength of glenohumeral and scapular muscles
- Improve neuromuscular control of shoulder complex
- Enhance proprioception and kinesthesia
Exercises:
- Initiate isotonic strengthening: IR/ER (sideling dumbbell), abduction to 90°
- Initiate eccentric exercises at 0° abduction, IR/ER
- Improve neuromuscular control of shoulder complex: Rhythmic stabilisation drills at inner, mid, and outer ROM, proprioceptive, scapulothoracic/glenohumeral musculature, PNF, weight shifts hand on ball, wall stabilisation drills.
Phase III: Advanced strengthening phase[edit | edit source]
Criteria to Progress to Phase III:
- Full pain-free ROM
- No pain or tenderness
- Continued progression of resistive exercises
- Good to normal muscle strength
Goals:
- Enhance dynamic stabilisation
- Improve strength/endurance
- Improve neuromuscular control
- Prepare patient for activity
Exercises:
- Continue isotonic strengthening
- Continue eccentric strengthening
- Emphasise PNF exercises with rhythmic stabilisation hold
- Continue to progress neuromuscular control drills: push-ups with rhythmic stabilisation, progress to unsteady surface, medicine ball, rocker board
- Program scapular neuromuscular control training: Sidelyng manual drills
- Emphasise endurance training: Timed sessions of exercise (30-60s), increasing number of reps
Phase IV - Return to activity phase[edit | edit source]
Goals:
- Maintain optimal level of strength/power/endurance
- Progressively increase activity level to prepare patient/athlete for full functional return to activity/sport
Exercises:
- Continue all exercises as in phase III
- Initiate interval sport program
- Patient education
Criteria to Progress to Phase IV:
- Full ROM
- No pain or palpable tenderness
- Satisfactory isokinetic test
- Satisfactory clinical exam
Clinical Bottom Line[edit | edit source]
- Shoulder instability may have a traumatic or atraumatic cause.
- Anterior shoulder instability is an injury to the shoulder joint so that the upper arm is displaced from its normal position in glenoid and the joint surfaces no longer contact each other.
- Anterior shoulder dislocations are much more common than posterior dislocations.
- The recurrence rate after primary shoulder dislocation is greatest in individuals less than 20 years old. Anterior instability accounts for 95% of acute traumatic dislocations.
- Diagnosis of anterior shoulder instability is made through history, radiology and the following three tests: apprehension, relocation and surprise (release) test, performed respectively.
- Rehabilitation should be based on an individual basis with consideration to the patient’s pre-morbid state and level of activity.
References:[edit | edit source]
- ↑ Medscape. Anterior Glenohumeral Instability. Available from: https://emedicine.medscape.com/article/1262004-overview (accessed 29 August 2020).
- ↑ Web MD. Picture of the shoulder. Available from: http://www.webmd.com/pain-management/picture-of-the-shoulder (accessed 29 August 2020).
- ↑ 3.0 3.1 3.2 Chen AL, Bosco III JA. Glenohumeral bone loss and anterior instability. Bulletin of the NYU hospital for joint diseases 2006 Dec 22;64(3-4):130-138.
- ↑ 4.0 4.1 4.2 Araghi A, Prasarn M, St Clair S, Zuckerman JD. Recurrent anterior glenohumeral instability with onset after forty years of age. Bull Hosp Joint Dis 2005 Jan 1;62:99-101.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Pope EJ, Ward JP, Rokito AS. Anterior shoulder instability - a history of arthroscopic treatment. Bull NYU Hosp Jt Dis 2011;69(1):44-9.
- ↑ Rhee YG, Lim CT. Glenoid defect associated with anterior shoulder instability: results of open Bankart repair. Int Orthop 2007;31(5):629-34.
- ↑ 7.0 7.1 7.2 7.3 7.4 Satterwhite YE. Evaluation and management of recurrent anterior shoulder instability. Journal of athletic training 2000 Jul;35(3):273.
- ↑ 8.0 8.1 Lo IK, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. The American Journal of Sports Medicine 2004;32(2):301-7.
- ↑ 9.0 9.1 Dumont GD, Russell RD, Robertson WJ. Anterior shoulder instability: a review of pathoanatomy, diagnosis and treatment. Current reviews in musculoskeletal medicine 2011;4(4):200.
- ↑ Pavlov H, Warren RF, Weiss Jr CB, Dines DM. The roentgenographic evaluation of anterior shoulder instability. Clinical Orthopaedics and Related Research 1985;194:153-8.
- ↑ Rokous JR, Feagin JA, Abbott HG. Modified axillary roentgenogram a useful adjunct in the diagnosis of recurrent instability of the shoulder. Clinical Orthopaedics and Related Research 1972;82:84-6.
- ↑ Shultz SJ, Houglum PA, Perrin DH. Examination of musculoskeletal injuries. Human Kinetics; 2005.
- ↑ 13.0 13.1 Farber AJ, Castillo R, Clough M, Bahk M, McFarland EG. Clinical assessment of three common tests for traumatic anterior shoulder instability. JBJS 2006;88(7):1467-74.
- ↑ Savoie III FH, O’Brien MJ. Anterior instability in the throwing shoulder. Sports Medicine and Arthroscopy Review 2014;22(2):117-9.
- ↑ Milgrom C, Milgrom Y, Radeva-Petrova D, Jaber S, Beyth S, Finestone AS. The supine apprehension test helps predict the risk of recurrent instability after a first-time anterior shoulder dislocation. Journal of shoulder and elbow surgery 2014;23(12):1838-42.
- ↑ Wilson SR, Price DD. Shoulder Dislocation in Emergency Medicine. Medscape; 2011.
- ↑ 17.0 17.1 Wilk KE, Macrina LC, Reinold MM. Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability. North American journal of sports physical therapy 2006;1(1):16.
- ↑ 18.0 18.1 Burkhead Jr WZ, Rockwood Jr CA. Treatment of instability of the shoulder with an exercise program. JBJS 1992;74(6):890-6.