Dysarthria: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 62: | Line 62: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Various dysarthria types, for instance, ataxic, hyperkinetic, and unilateral upper motor neuron may apportion some characteristics with Apraxia of Speech and can be difficult to differentiate<ref>Bislick L, McNeil M, Spencer KA, Yorkston K, Kendall DL. [https://pubs.asha.org/doi/abs/10.1044/2017_AJSLP-16-0080 The nature of error consistency in individuals with acquired apraxia of speech and aphasia.] American Journal of Speech-Language Pathology. 2017 Jun 22;26(2S):611-30.</ref>. One comparison is the presence or absence of muscle weakness or spasticity. Apraxia of Speech does not extant with muscle weakness or spasticity unless there is a concurrent dysarthria<ref name=":1" />. | |||
Aphasia impacts language discernment and expression in both spoken and written formats; dysarthria impacts only speech creation. Therefore, assessment of written language expression in conjunction with assessment of written language understanding may be warranted to make a conclusive diagnosis<ref name=":1" />. | |||
= | Finally, Speech and Language Therapists will assess the effect of culture and linguistic components on the patient's communication manner and the possible ramifications of ailment on function. Diversifications in dialect should be taken into account prior marking linguistics in error, as they may not have been part of the patient's spoken language or dialect initially to the injury or disease<ref name=":1" />. | ||
[https://www.asha.org/ | == Resources == | ||
[https://www.asha.org/Practice-Portal/Clinical-Topics/Dysarthria-in-Adults/ American Speech-Language-Hearing Association] | |||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 15:40, 9 November 2020
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (26/10/2020)[edit | edit source]
Introduction[edit | edit source]
Dysarthria pertains to a category of neurogenic speech disorders distinguished by an anomaly in the strength, speed, availability, stableness, tone, or accuracy of movements necessary for breathing, phonatory, resonatory, articulatory, or prosodic features of speech creation[1].
These anomalies are the result of one or several sensorimotor issues, including weakness or paralysis, incoordination, involuntary movements, or immoderate, declined, or inconstant muscle tone[1]. Dysarthria can negatively impact the comprehensibility of speech, realism of speech, or both. It is necessary to be aware that intelligence can be normal in some speakers with dysarthria. Dysarthria might co-exist with other neurogenic language, cognitive, and swallowing disorders[2].
Mechanism of Injury / Pathological Process[edit | edit source]
Damage to the nervous system causes hypotonicity in the muscles that create speech sounds. This may impact the muscles in one or several of the following areas:
- Face
- Lips
- Tongue
- Throat
- Upper respiratory tract
The neurological damage that can result in dysarthria can be from[1]:
- Congenital: cerebral palsy, Chiari malformation, congenital suprabulbar palsy, syringomyelia, syringobulbia.
- Degenerative diseases: amyotrophic lateral sclerosis (ALS), Parkinson's disease, progressive supranuclear palsy, cerebellar degeneration, corticobasal degeneration, multiple system atrophy, Friedreich's ataxia, Huntington's disease, olivopontocerebellar atrophy, spinocerebellar ataxia, ataxia telangiectasia.
- Demyelinating and inflammatory diseases: multiple sclerosis, encephalitis, Guillain-Barré and associated autoimmune diseases,meningitis, multifocal leukoencephalopathy.
- Infectious diseases: acquired immune deficiency syndrome (AIDS), Creutzfeldt-Jakob disease, herpes zoster, infectious encephalopathy, central nervous system tuberculosis, poliomyelitis.
- Neoplastic diseases: central nervous system tumors; cerebral, cerebellar, or brainstem tumors; paraneoplastic cerebellar degeneration.
- Other neurologic conditions: hydrocephalus, Meige syndrome, myoclonic epilepsy, neuroacanthocytosis, radiation necrosis, sarcoidosis, seizure disorder, Tourette's syndrome, Chorea gravidarum
- Toxic/metabolic diseases: alcohol, botulism, carbon monoxide poisoning, central pontine myelinolysis, heavy metal or chemical toxicity, hepatocerebral degeneration, hypothyroidism, hypoxic encephalopathy, lithium toxicity, Wilson's disease.
- Trauma: traumatic brain injury, chronic traumatic encephalopathy, neck trauma, neurosurgical/postoperative trauma, skull fracture.
- Vascular Diseases: stroke (hemorrhagic or nonhemorrhagic), Moyamoya disease, anoxic or hypoxic encephalopathy, arteriovenous malformations.
Incidence and Prevalence[2][edit | edit source]
- Stroke: Estimated that 8%–60% of patients with stroke present with dysarthria.
- Traumatic brain injury: Approximately 10%–65% of patients post traumatic brain injury have dysarthria.
- Parkinson's disease: Estimation that dysarthria impacts approximately 70%–100% of patients post Parkinson's disease.
- Multiple sclerosis: Amidst 25% and 50% of patients with multiple sclerosis show with dysarthria at some stage during the continuity of their disease.
- Amyotrophic lateral sclerosis: Dysarthria can be seen as an initial symptom in up to 30% of patients with this condition, with relatively all patients developing dysarthria in later stages.
Clinical Presentation[edit | edit source]
Depending on the location of the neurological damage different types of dysarthria have been described;
- Flaccid: affiliated with conditions of the lower motor neuron system and/or muscle, for instance damage to the peripheral nervous system (PNS). Hallmarked by difficulty pronouncing consonants.
- Spastic: affiliated with bilateral illnesses of the upper motor neuron system. Patients may have speech issues alongside muscle weakness and abnormal reflexes.
- Ataxic: affiliated with conditions of the cerebellar control unit. Symptoms of slurred speech and lack of coordination.
- Hypokinetic: affiliated with infirmity of the basal ganglia control unit, such as insult caused by neurodegenerative diseases, such as Parkinson’s and Huntington’s. Presents as quiet, breathy, or monotone voice, difficulty initiating sentences, a stutter or slurred speech, struggles pronouncing consonants, rigidity or lacked movement in the face and neck, swallow difficulty that can result in drooling and tremors or muscle spasms.
- Hyperkinetic: affiliated with ailment of the basal ganglia control unit. Symptoms include slurred or slow speech, shaky voice, shortness of breath or fatigue while speaking, muscle spasms and tremors, involuntary twitchy or flailing movements or atypical muscle tone.
- Unilateral upper motor neuron: affiliated with unilateral disorders of the upper motor neuron system
- Mixed: variety blend of dysarthria types (for example spastic-ataxic; flaccid-spastic)
- Undetermined: observed features are in line with a dysarthria but do not clearly place into any of the identified dysarthria types[2][3].
Diagnostic Procedures[edit | edit source]
Physiotherapists treating patients with neurogenic type conditions, may assist in screening for dysarthria. This screening is not required to give a diagnosis or a specific narration of the severity and features of speech deficits affiliated with dysarthria but, rather, highlights the need for additional assessment. Assessment of patients with suspected dysarthria should be performed by a Speech and Language Therapist.
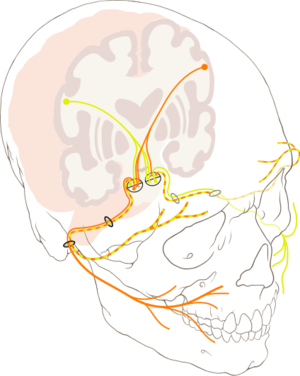
Objective measures that a physiotherapist could assess, and are included as a component in the non-speech examination;
- Completion of a cranial nerve exam (CN V, VII, IX, X, XI, XII)—to examine facial, oral, velopharyngeal, and laryngeal function and symmetry
- Observation of facial and neck muscle tone, both at rest and during non-speech activities[4].
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis[edit | edit source]
Various dysarthria types, for instance, ataxic, hyperkinetic, and unilateral upper motor neuron may apportion some characteristics with Apraxia of Speech and can be difficult to differentiate[5]. One comparison is the presence or absence of muscle weakness or spasticity. Apraxia of Speech does not extant with muscle weakness or spasticity unless there is a concurrent dysarthria[2].
Aphasia impacts language discernment and expression in both spoken and written formats; dysarthria impacts only speech creation. Therefore, assessment of written language expression in conjunction with assessment of written language understanding may be warranted to make a conclusive diagnosis[2].
Finally, Speech and Language Therapists will assess the effect of culture and linguistic components on the patient's communication manner and the possible ramifications of ailment on function. Diversifications in dialect should be taken into account prior marking linguistics in error, as they may not have been part of the patient's spoken language or dialect initially to the injury or disease[2].
Resources[edit | edit source]
American Speech-Language-Hearing Association
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Duffy JR. Motor Speech Disorders: Substrates, Differential Diagnosis, and Management, 3rd edn. St. Louis, MO: Elsevier, Mosby. 2013.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 American Speech-Language-Hearing Association. Dysarthria in Adults. Available from: https://www.asha.org/PRPSpecificTopic.aspx?folderid=8589943481§ion=Overview [accessed 26 October 2020].
- ↑ Medical News Today. What to know about dysarthria. Available from: https://www.medicalnewstoday.com/articles/327362 [last accessed 27/10/2020].
- ↑ Clark HM, Solomon NP. Muscle tone and the speech-language pathologist: Definitions, neurophysiology, assessment, and interventions. Perspectives on Swallowing and Swallowing Disorders (Dysphagia). 2012 Mar;21(1):9-14.
- ↑ Bislick L, McNeil M, Spencer KA, Yorkston K, Kendall DL. The nature of error consistency in individuals with acquired apraxia of speech and aphasia. American Journal of Speech-Language Pathology. 2017 Jun 22;26(2S):611-30.