Graves' Disease: Difference between revisions
No edit summary |
m (Lucinda hampton moved page Grave's Disease to Graves' Disease: corrected spelling) |
||
| (One intermediate revision by the same user not shown) | |||
| Line 6: | Line 6: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
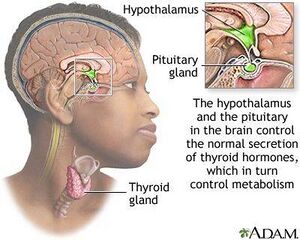
[[File:Proptosis and lid retraction from Graves' Disease.jpeg|thumb|Classic finding: Graves' Disease-proptosis and lid retraction.|alt=]]Graves’ disease (GD), the most common cause of [[hyperthyroidism]], is an autoimmune | [[File:Proptosis and lid retraction from Graves' Disease.jpeg|thumb|Classic finding: Graves' Disease-proptosis and lid retraction.|alt=]]Graves’ disease (GD), the most common cause of [[hyperthyroidism]], is an [[Autoimmune Disorders|autoimmune disorder]] that affects the [[Thyroid Gland|thyroid gland]]. Graves’ disease causes the immune system to attack the thyroid, leading to excess thyroid hormone production. The treatment is relatively simple, but without it, the disease can have serious effects. Failure to diagnose Graves' disease can predispose [[Thyroid Storm (Thyroid Crisis)|thyroid storm]] which carries high morbidity and mortality<ref name=":0">Pokhrel B, Bhusal K. [https://www.ncbi.nlm.nih.gov/books/NBK448195/ Graves disease]. StatPearls [Internet]. 2021 Jul 21.Available: https://www.ncbi.nlm.nih.gov/books/NBK448195/<nowiki/>(accessed 23.2.2022)</ref>. | ||
Graves' disease primarily affects the thyroid gland but may also affect multiple other organs including eyes and skin.<ref name=":0" />. | Graves' disease primarily affects the thyroid gland but may also affect multiple other organs including eyes and skin.<ref name=":0" />. | ||
== Etiology == | == Etiology == | ||
Like all autoimmune diseases, it occurs more commonly in patients with a positive family history. It is precipitated by environmental factors eg stress, smoking, infection, iodine exposure, and postpartum, as well as after highly active antiretroviral therapy (HAART) due to immune reconstitution.<ref name=":0" /> | [[File:Thyroid and release.jpeg|thumb|Thyroid function]] | ||
Like all autoimmune diseases, it occurs more commonly in patients with a positive family history. It is precipitated by environmental factors eg [[Stress and Health|stress]], [[Smoking Cessation and Brief Intervention|smoking]], [[Infectious Disease|infection]], iodine exposure, and postpartum, as well as after highly active [[Antiviral Drugs|antiretroviral therapy]] (HAART) due to immune reconstitution.<ref name=":0" /> | |||
Having another autoimmune condition may also increase the risk of Graves’ disease. Some of these conditions include: rheumatoid arthritis; pernicious anemia; lupus; Addison’s disease; celiac disease; | Having another autoimmune condition may also increase the risk of Graves’ disease. Some of these conditions include: [[Rheumatoid Arthritis|rheumatoid arthritis]]; pernicious [[anemia]]; [[Systemic Lupus Erythematosus|lupus]]; [[Addison's Disease|Addison’s disease]]; [[Celiac Disease (Coeliac Disease)|celiac]] disease; [[Diabetes Mellitus Type 1|type 1 diabetes]].<ref name=":1" /> | ||
== Clinical Presentation == | == Clinical Presentation == | ||
The overproduction of thyroid | The overproduction of thyroid [[Hormones|hormone]]<nowiki/>s can have a variety of effects on the body. Symptoms can include: intolerance to heat; unexplained weight loss; nervousness; sweating; hand tremors; difficulty sleeping; tiredness or weakness; irritability; frequent bowel movements or diarrhea; a goiter (an enlarged thyroid gland); an irregular or rapid heartbeat. | ||
In rare cases, Graves’ disease can lead to Graves’ dermopathy, which causes thick, flushed skin on the shins<ref name=":1">Medical news Today [https://www.medicalnewstoday.com/articles/170005#symptoms Graves Disease] Available:https://www.medicalnewstoday.com/articles/170005#symptoms (accessed 23.2.2022)</ref>.<ref name="Pathology" /> | In rare cases, Graves’ disease can lead to Graves’ dermopathy, which causes thick, flushed skin on the shins<ref name=":1">Medical news Today [https://www.medicalnewstoday.com/articles/170005#symptoms Graves Disease] Available:https://www.medicalnewstoday.com/articles/170005#symptoms (accessed 23.2.2022)</ref>.<ref name="Pathology">Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier; 2009.</ref> | ||
== Diagnosis == | == Diagnosis == | ||
[[File:Thyroid Gland- location.png|thumb]] | |||
Diagnosis of Graves disease starts with a thorough history and physical examination. History should include a family history of Graves’ disease. | Diagnosis of Graves disease starts with a thorough history and physical examination. History should include a family history of Graves’ disease. | ||
The medical team may order: | The medical team may order: | ||
# Thyroid function tests to diagnose hyperthyroidism. The initial test is the a blood test for thyroid-stimulating hormone (TSH)<ref name=":0" />. | # Thyroid function tests to diagnose hyperthyroidism. The initial test is the a [[Blood Tests|blood test]] for thyroid-stimulating hormone (TSH)<ref name=":0" />. | ||
# A radioactive iodine uptake test, which measures how much iodine the thyroid gland gathers from the bloodstream | # A radioactive iodine uptake test, which measures how much iodine the thyroid gland gathers from the [[Blood Physiology|bloodstream]] | ||
# A thyroid scan, to show how much iodine is in the thyroid gland. High levels of iodine may indicate Graves’ disease.<ref name=":1" /> | # A thyroid scan, to show how much iodine is in the thyroid gland. High levels of iodine may indicate Graves’ disease.<ref name=":1" /> | ||
| Line 35: | Line 34: | ||
* Antithyroid drug use can cause drug-induced embryopathy in pregnancy, | * Antithyroid drug use can cause drug-induced embryopathy in pregnancy, | ||
* Radioiodine therapy can exacerbate | * Radioiodine therapy can exacerbate graves' orbitopathy | ||
* Surgery can result in hypoparathyroidism or laryngeal nerve damage. | * Surgery can result in hypoparathyroidism or laryngeal nerve damage. | ||
| Line 42: | Line 41: | ||
# Antithyroid drugs: These medications work to reduce the amount of hormone that the thyroid makes. This is one of the simplest approaches hyperthyroidism<ref name=":1" />. | # Antithyroid drugs: These medications work to reduce the amount of hormone that the thyroid makes. This is one of the simplest approaches hyperthyroidism<ref name=":1" />. | ||
# Radioiodine therapy: involves taking radioactive iodine orally, either in capsule or liquid form. It targets the thyroid gland and destroys the cells that produce thyroid hormone. This means that most people who have radioiodine therapy go on to develop hypothyroidism. This is much easier to manage and does not cause as many long-term health issues as hyperthyroidism.<ref name=":1" /> | # Radioiodine therapy: involves taking radioactive iodine orally, either in capsule or liquid form. It targets the thyroid gland and destroys the cells that produce thyroid hormone. This means that most people who have radioiodine therapy go on to develop hypothyroidism. This is much easier to manage and does not cause as many long-term health issues as hyperthyroidism.<ref name=":1" /> | ||
== Physical Therapy Management == | == Physical Therapy Management == | ||
Graves' disease is not directly managed by physical therapy but precautions and understanding of the disease are necessary when working with these patients. Deconditioning and muscle weakness are secondary ailments that is seen in this population and can be managed by a physical therapist.<ref name="Pathology" /> | Graves' disease is not directly managed by physical therapy but precautions and understanding of the disease are necessary when working with these patients. Deconditioning and muscle weakness are secondary ailments that is seen in this population and can be managed by a physical therapist.<ref name="Pathology" /> | ||
Hyperthyroidism has key elements that will cause a decreased tolerance to physical activity. Therapists should be sensitive to patient complaints and symptoms to note an exacerbation if the patient is already diagnosed or be able to recognize symptoms in order to refer to a physician.<ref name="DD">Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, Missouri: Saunders Elsevier, 2007.</ref> | |||
Hyperthyroidism has key elements that will cause a decreased tolerance to physical activity. Therapists should be sensitive to patient complaints and symptoms to note an exacerbation if the patient is already diagnosed or be able to recognize symptoms in order to refer to a physician.<ref name="DD" /> | |||
=== Precautions for Graves Related Hyperthyroidism === | === Precautions for Graves Related Hyperthyroidism === | ||
| Line 130: | Line 82: | ||
<ref name="DD" /><ref name="Pathology" /><ref name="Fukushima">Fukushima H, Matsuo H, Imamura K, et al. Diagnosis and discrimination of autoimmune graves’ diseas nad Hashimoto’s disease using thyroid stimulation hormone receptor-containing recombinant proteoliposomes. Journal of Bioscience and Bioengineering. 2009. 108(6):551-56.</ref> | <ref name="DD" /><ref name="Pathology" /><ref name="Fukushima">Fukushima H, Matsuo H, Imamura K, et al. Diagnosis and discrimination of autoimmune graves’ diseas nad Hashimoto’s disease using thyroid stimulation hormone receptor-containing recombinant proteoliposomes. Journal of Bioscience and Bioengineering. 2009. 108(6):551-56.</ref> | ||
== References == | == References == | ||
Latest revision as of 01:36, 26 February 2022
Original Editors - Erin Shinkle from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Erin Shinkle, Elaine Lonnemann, Lucinda hampton, Admin, Kim Jackson, WikiSysop, Wendy Walker and Andeela Hafeez
Introduction[edit | edit source]
Graves’ disease (GD), the most common cause of hyperthyroidism, is an autoimmune disorder that affects the thyroid gland. Graves’ disease causes the immune system to attack the thyroid, leading to excess thyroid hormone production. The treatment is relatively simple, but without it, the disease can have serious effects. Failure to diagnose Graves' disease can predispose thyroid storm which carries high morbidity and mortality[1].
Graves' disease primarily affects the thyroid gland but may also affect multiple other organs including eyes and skin.[1].
Etiology[edit | edit source]
Like all autoimmune diseases, it occurs more commonly in patients with a positive family history. It is precipitated by environmental factors eg stress, smoking, infection, iodine exposure, and postpartum, as well as after highly active antiretroviral therapy (HAART) due to immune reconstitution.[1]
Having another autoimmune condition may also increase the risk of Graves’ disease. Some of these conditions include: rheumatoid arthritis; pernicious anemia; lupus; Addison’s disease; celiac disease; type 1 diabetes.[2]
Clinical Presentation[edit | edit source]
The overproduction of thyroid hormones can have a variety of effects on the body. Symptoms can include: intolerance to heat; unexplained weight loss; nervousness; sweating; hand tremors; difficulty sleeping; tiredness or weakness; irritability; frequent bowel movements or diarrhea; a goiter (an enlarged thyroid gland); an irregular or rapid heartbeat.
In rare cases, Graves’ disease can lead to Graves’ dermopathy, which causes thick, flushed skin on the shins[2].[3]
Diagnosis[edit | edit source]
Diagnosis of Graves disease starts with a thorough history and physical examination. History should include a family history of Graves’ disease.
The medical team may order:
- Thyroid function tests to diagnose hyperthyroidism. The initial test is the a blood test for thyroid-stimulating hormone (TSH)[1].
- A radioactive iodine uptake test, which measures how much iodine the thyroid gland gathers from the bloodstream
- A thyroid scan, to show how much iodine is in the thyroid gland. High levels of iodine may indicate Graves’ disease.[2]
Treatment[edit | edit source]
The treatment of GD has not changed substantially for many years and remains a choice between antithyroid drugs, radioiodine or surgery. However:
- Antithyroid drug use can cause drug-induced embryopathy in pregnancy,
- Radioiodine therapy can exacerbate graves' orbitopathy
- Surgery can result in hypoparathyroidism or laryngeal nerve damage.
Future studies should focus on improved drug management, and a number of important advances are on the horizon[4].
- Antithyroid drugs: These medications work to reduce the amount of hormone that the thyroid makes. This is one of the simplest approaches hyperthyroidism[2].
- Radioiodine therapy: involves taking radioactive iodine orally, either in capsule or liquid form. It targets the thyroid gland and destroys the cells that produce thyroid hormone. This means that most people who have radioiodine therapy go on to develop hypothyroidism. This is much easier to manage and does not cause as many long-term health issues as hyperthyroidism.[2]
Physical Therapy Management [edit | edit source]
Graves' disease is not directly managed by physical therapy but precautions and understanding of the disease are necessary when working with these patients. Deconditioning and muscle weakness are secondary ailments that is seen in this population and can be managed by a physical therapist.[3]
Hyperthyroidism has key elements that will cause a decreased tolerance to physical activity. Therapists should be sensitive to patient complaints and symptoms to note an exacerbation if the patient is already diagnosed or be able to recognize symptoms in order to refer to a physician.[5]
Precautions for Graves Related Hyperthyroidism[edit | edit source]
- Decreased Cardiorespiratory function causing dyspnea on exertion and tachycardia
- Palpitations/Atrial Fibrillation (therefore therapist should be monitoring vital signs and symptoms)
- Decreased efficiency of oxygen uptake in peripheral musculature
- Heat intolerance is seen in Grave's disease
- Myopathies and proximal muscle weakness
All of these are reversible with the management of thyroid hormones and acheivement of Euthyroid. [5][6]
The therapist should have a base knowledge and understanding of the medication and or surgeries that these patients have undergone. The reasons are as follows:
- Medications can fluctuate the thyroid hormones to either send the patient into Hypothyroidism or Hyperthyroidism. It is imperative to watch for symptoms or patient complaints that may indicate a fluctuation and refer the patient back to their endocrinologist since these two extremes will vary tolerance for physical activity.[5][3]
- If a patient has recently had surgery or radioiodine treatment it is possible that you will see hypothyroidism.[7]
- If a patient is on Beta-blockers for management tremors, anxiety, and palpitations during the exacerbation period, the therapist must be aware fo the physiological effects this can have on a patient during physical therapy.[7]Therefore, a better measurement of vitals is the rate of perceived exertion.[3]
Precautions/Symptoms Related to Hypothyroidism[edit | edit source]
If the patient is on medication or is post-surgical there are certain things that need to be taken into consideration: [3]
- Excessive fatigue and apathy
- Sensitivity to cold
- Weight gain/ dry brittle hair/ and other
- Decreased cardiac output, low pulse and poor circulation
- Ataxia, intention tremor, and nystagmus
Differential Diagnosis[edit | edit source]
- Hyperthyroidism
- Thyroid Storm
- Hyperparathyroidism
- Thyroid cancer
- Myasthenia gravis
- Psychological disorders (anxiety, panic attacks, or mood disorders)
- Atrial Fibrillation
- Congestive Heart Failure
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Pokhrel B, Bhusal K. Graves disease. StatPearls [Internet]. 2021 Jul 21.Available: https://www.ncbi.nlm.nih.gov/books/NBK448195/(accessed 23.2.2022)
- ↑ 2.0 2.1 2.2 2.3 2.4 Medical news Today Graves Disease Available:https://www.medicalnewstoday.com/articles/170005#symptoms (accessed 23.2.2022)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier; 2009.
- ↑ Davies TF, Andersen S, Latif R, Nagayama Y, Barbesino G, Brito M, Eckstein AK, Stagnaro-Green A, Kahaly GJ. Graves’ disease. Nature reviews Disease primers. 2020 Jul 2;6(1):1-23.Available: https://pubmed.ncbi.nlm.nih.gov/32616746/(accessed 24.2.2022)
- ↑ 5.0 5.1 5.2 5.3 Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, Missouri: Saunders Elsevier, 2007.
- ↑ Mercuro G, Panzuto MG, Bina A, et al. Cardiac function, physical exercise Capacity, and quality of Life during long term thyrotropin-suppressive therapy with Levothyroxine: Effect of individual Dose Tailoring. J of Clinical endocrinology and metabolism. 2000 85: 159-164.
- ↑ 7.0 7.1 Franklyn J. The management of Hyperthyroidism. New England Journal of Medicine. 1994; 331(8):559.
- ↑ Fukushima H, Matsuo H, Imamura K, et al. Diagnosis and discrimination of autoimmune graves’ diseas nad Hashimoto’s disease using thyroid stimulation hormone receptor-containing recombinant proteoliposomes. Journal of Bioscience and Bioengineering. 2009. 108(6):551-56.