Hill Sachs Lesion: Difference between revisions
Leana Louw (talk | contribs) No edit summary |
No edit summary |
||
| (27 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Lien Hennebel|Lien Hennebel]] | '''Original Editors ''' - [[User:Lien Hennebel|Lien Hennebel]] as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Description == | |||
A Hill-Sachs lesion is an osseous defect or "dent" of the postero-supero-lateral humeral head that occurs in association with [[Anterior Shoulder Instability|anterior instability]] or [[Shoulder Dislocation|dislocation of the glenohumeral joint]].<ref name="provencher">Provencher MT, Frank RM, LeClere LE, Metzger PD, Ryu JJ, Bernhardson A, Romeo AA. [https://journals.lww.com/jaaos/Abstract/2012/04000/The_Hill_Sachs_Lesion__Diagnosis,_Classification,.11.aspx The Hill-Sachs lesion: diagnosis, classification, and management.] Journal of the American Academy of Orthopaedic Surgeons 2012;20(4):242-52.</ref><ref name=":0">Shoulder Doc. Hill-Sachs Lesion. Available from: https://www.shoulderdoc.co.uk/article/1470 (accessed 24 December 2023).</ref> It is often associated with a [[Bankart lesion]] of the glenoid.<ref name=":2">Radiopedia [https://radiopaedia.org/articles/hill-sachs-defect?lang=gb Hills Sachs defect] Available from:https://radiopaedia.org/articles/hill-sachs-defect?lang=gb (accessed 24 December 2023)</ref> This lesion is caused by an anterior shoulder dislocation which causes a humeral head impression fracture. The posterolateral aspect of the humeral head impacts on the anterior [[Glenoid Labrum|glenoid]] in the dislocated position, causing [[Shoulder Instability|shoulder instability]].<ref name="provencher 2">Provencher MT, Frank RM, Leclere LE, Metzger PD, Ryu JJ, Bernhardson A, Romeo AA. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012 Apr;20(4):242-52. doi: 10.5435/JAAOS-20-04-242. </ref><ref name="castro">Castro WHM, Jerosch J, Grossman TV. Examination and diagnosis of musculoskeletal disorders. Georg Thieme Verlag: Germany, 2001.</ref><ref name="dodson">Dodson CC, Cordasco FA. [https://www.sciencedirect.com/science/article/pii/S0030589808000461 Anterior glenohumeral joint dislocations.] Orthopedic Clinics of North America 2008;39(4):507-18.</ref> | |||
== | Watch this animated description of Hill-Sachs and [[Bankart lesion|Bankart Lesions]] that can occur with a shoulder dislocation and contribute to further shoulder instability (2 minutes) | ||
{{#ev:youtube|v=a6BWiufgmsc|300}}<ref> ORTHOfilms. Bankart and Hill-Sachs Lesions. Available from: https://www.youtube.com/watch?v=a6BWiufgmsc [last accessed 10.1.2023]</ref> | |||
== Epidemiology == | |||
The incidence of Hill-Sachs lesions are approximately 40%-90% of all anterior shoulder instability cases, and even as high as 100% in patients with recurrent anterior instability.<ref name="provencher" /> A study looking at this found Hill-Sachs lesions in 65% of acute dislocations and 93% in patients with recurrent instability.<ref name="christos">Yiannakopoulos CK, Mataragas E, Antonogiannakis E. [http://www.orthosurgery.gr/dimosieusis/AComparisonoftheSpectrumofIntra-articularLesionsinAcuteandChronicAnteriorShoulderInstability.pdf A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability.] Arthroscopy: The Journal of Arthroscopic & Related Surgery 2007;23(9):985-90.</ref><br>A Hill-Sachs lesion occurs in about 50% of the first-time shoulder dislocations. For people with a shoulder dislocations history (i.e. shoulder instability) humeral head compression fractures are present in most cases.<ref name="fuller" /> | |||
== Etiology == | |||
== Epidemiology | |||
The incidence of Hill-Sachs lesions are approximately 40%-90% of all | |||
A Hill-Sachs lesion occurs in about 50% of the first-time shoulder dislocations. For people with a shoulder dislocations history (i.e. shoulder instability) humeral head compression fractures are present in most cases.<ref name="fuller" / | |||
* [http://www.physio-pedia.com/Anterior_Shoulder_Instability Anterior shoulder instability]: | * [http://www.physio-pedia.com/Anterior_Shoulder_Instability Anterior shoulder instability]: | ||
** Approximately 47% of the lesions are associated with the initial shoulder instability according to research studies | ** Approximately 47% of the lesions are associated with the initial shoulder instability according to research studies<ref name="calandra">Calandra JJ, Baker CL, Uribe J. [https://www.sciencedirect.com/science/article/pii/0749806389901382 The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations.] Arthroscopy: The Journal of Arthroscopic & Related Surgery 1989;5(4):254-7.</ref> | ||
* [http://www.physio-pedia.com/Bankart_lesion Bankart lesion]<ref name="horst">Horst K, Von Harten R, Weber C, Andruszkow H, Pfeifer R, Dienstknecht T, | * [http://www.physio-pedia.com/Bankart_lesion Bankart lesion]<ref name="horst">Horst K, Von Harten R, Weber C, Andruszkow H, Pfeifer R, Dienstknecht T, et al. [https://www.birpublications.org/doi/pdfplus/10.1259/bjr.20130673 Assessment of coincidence and defect sizes in Bankart and Hill–Sachs lesions after anterior shoulder dislocation: a radiological study.] The British journal of radiology 2014;87(1034):20130673.</ref> | ||
** 2.5 times more likely to for someone with either of those lesions to have the other as well<ref name="widjadja">Widjaja AB, Tran A, Bailey M, Proper S. [https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1445-2197.2006.03760.x Correlation between Bankart and Hill‐Sachs lesions in anterior shoulder dislocation.] ANZ journal of surgery | ** 2.5 times more likely to for someone with either of those lesions to have the other as well<ref name="widjadja">Widjaja AB, Tran A, Bailey M, Proper S. [https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1445-2197.2006.03760.x Correlation between Bankart and Hill‐Sachs lesions in anterior shoulder dislocation.] ANZ journal of surgery 2006;76(6):436-8.</ref> | ||
* Anterior glenoid bone loss (in cases of recurrent instability)<ref name="kim">Kim DS, Yoon YS, Yi CH. [http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.858.1952&rep=rep1&type=pdf Prevalence comparison of accompanying lesions between primary and recurrent anterior dislocation in the shoulder.] The American journal of sports medicine | * Anterior glenoid bone loss (in cases of recurrent instability)<ref name="kim">Kim DS, Yoon YS, Yi CH. [http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.858.1952&rep=rep1&type=pdf Prevalence comparison of accompanying lesions between primary and recurrent anterior dislocation in the shoulder.] The American journal of sports medicine 2010;38(10):2071-6.</ref> | ||
== Classification == | |||
Classification systems are used to describe the amount of damage to the anterior capsule and the labrum, reflected by the depth of the lesion. Higher grade lesions are associated with increased risk of recurrent dislocation.<ref name="provencher" /><ref name=":0" /><ref name="calandra" /> | Classification systems are used to describe the amount of damage to the anterior capsule and the labrum, reflected by the depth of the lesion. Higher grade lesions are associated with increased risk of recurrent dislocation.<ref name="provencher" /><ref name=":0" /><ref name="calandra" /> | ||
*'''Grade 1:''' Defect in the articular surface down to (but not including) the subchondral bone | *'''Grade 1:''' Defect in the articular surface down to (but not including) the subchondral bone | ||
| Line 77: | Line 27: | ||
*'''Grade 3:''' Lesion causes large defect in the subchondral bone. | *'''Grade 3:''' Lesion causes large defect in the subchondral bone. | ||
Further classification can be done by looking at the percentage of the defect of humeral head involvement in the compression fracture.<ref name="cetik">Cetik O, Uslu M, Ozsar BK. [http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.627.9326&rep=rep1&type=pdf The relationship between Hill-Sachs lesion and recurrent anterior shoulder dislocation.] Acta orthopaedica belgica | Further classification can be done by looking at the percentage of the defect of humeral head involvement in the compression fracture.<ref name="cetik">Cetik O, Uslu M, Ozsar BK. [http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.627.9326&rep=rep1&type=pdf The relationship between Hill-Sachs lesion and recurrent anterior shoulder dislocation.] Acta orthopaedica belgica 2007;73(2):175-8.</ref> The size of the lesion correlates in most cases to the number of previous dislocations.<ref name="savoie">Fox JA, Sanchez A, Zajac TJ, Provencher MT. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5685959/ Understanding the Hill-Sachs Lesion in Its Role in Patients with Recurrent Anterior Shoulder Instability.] Curr Rev Musculoskelet Med. 2017 Dec;10(4):469-479. doi: 10.1007/s12178-017-9437-0. </ref> | ||
* '''Minor:''' <20% | * '''Minor:''' <20% | ||
* '''Moderate:''' 20%-45% | * '''Moderate:''' 20%-45% | ||
* '''Severe:''' >45% | * '''Severe:''' >45% | ||
Shoulder dislocation rarely occur isolated. It causes damage to different tissues surrounding the [[Glenohumeral Joint|glenohumeral joint]], such as ligaments, rotator cuff tendons, joint capsule as well as the bone and cartilage of the humeral head. This occurs when the round humeral head is forcibly impacted on the edge of the glenoid, which causes compression fractures in the humeral head. This forms a dimple structure on the articular surface of the humerus - a Hill-Sachs lesion.<ref name="cluett">Cluett J. Hill-Sachs Injury: Damage to the shoulder joint as result of dislocation. Orthopedics, 2013.</ref><ref name="ahmed">Radiopedia. Hill-Sachs lesion. https://radiopaedia.org/articles/hill-sachs-lesion (accessed 27/08/2018).</ref><ref name="fuller">Wiki Radiography. Hill-Sachs and Bankart lesion | Another classification - ON track or OFF track<ref>Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2014 Jan 1;30(1):90-8.</ref> | ||
If the Hill-Sachs lesion engages, it is called an “off-track” Hill-Sachs lesion; if it does not engage, it is an “on-track” lesion. | |||
== Clinical Presentation == | |||
Shoulder dislocation rarely occur isolated. It causes damage to different tissues surrounding the [[Glenohumeral Joint|glenohumeral joint]], such as ligaments, [[Rotator Cuff|rotator cuff]] tendons, joint capsule as well as the [[bone]] and [[cartilage]] of the humeral head. This occurs when the round humeral head is forcibly impacted on the edge of the glenoid, which causes compression fractures in the humeral head. This forms a dimple structure on the articular surface of the humerus - a Hill-Sachs lesion.<ref name="cluett">Cluett J. Hill-Sachs Injury: Damage to the shoulder joint as result of dislocation. Orthopedics, 2013.</ref><ref name="ahmed">Radiopedia. Hill-Sachs lesion. https://radiopaedia.org/articles/hill-sachs-lesion (accessed 27/08/2018).</ref><ref name="fuller">Wiki Radiography. Hill-Sachs and Bankart lesion. Available from:http://www.wikiradiography.net/page/Hill-Sachs+and+Bankart+Lesions (accessed 25 December 2023).</ref>This is always caused by dislocation, not only subluxation.<ref name="cluett" /> | |||
According to the page on [[Shoulder Dislocation|shoulder dislocations]], the following indicates an acute anterior glenohumeral dislocation: | According to the page on [[Shoulder Dislocation|shoulder dislocations]], the following indicates an acute anterior glenohumeral dislocation: | ||
| Line 90: | Line 45: | ||
* Humeral head palpable anteriorly | * Humeral head palpable anteriorly | ||
* All movements limited and painful | * All movements limited and painful | ||
* Coracoid process: Palpable fullness and positioned towards the axilla | * Coracoid process: Palpable fullness and positioned towards the axilla<span style="line-height: 1.5em;"></span> | ||
<span style="line-height: 1.5em;"></span> | |||
== Differential diagnosis == | == Differential diagnosis == | ||
* [http://www.physio-pedia.com/Bankart_lesion Bankart lesion]: | * [http://www.physio-pedia.com/Bankart_lesion Bankart lesion]: Also as a result of shoulder dislocation, and often goes together<ref name="fuller" /><ref name="ahmed" /> | ||
* Pseudo-Hill-Sachs lesion: It is normal that below the level of the coracoid, the humeral head normally flattens out, and should not be mistaken as a Hill-Sachs lesion<ref name="ahmed" /> | |||
* Pseudo-Hill-Sachs lesion: | |||
* Humeral avulsion fractures<ref name="savoie" /> | * Humeral avulsion fractures<ref name="savoie" /> | ||
* Mid capsular tears<ref name="savoie" /> | * Mid capsular tears<ref name="savoie" /> | ||
* Floating anterior capsule<ref name="savoie" /> | * Floating anterior capsule<ref name="savoie" /> | ||
* Reverse Hill-Sachs lesion: | * Reverse Hill-Sachs lesion: Lesion on the anterior-superior aspect of the humeral head as the result of a posterior shoulder dislocation<ref name="fuller" /><ref name="savoie" /><ref name="ahmed" /> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
=== Physical examination === | === Physical examination === | ||
* [[Apprehension Test|Bony apprehension test]]: | * [[Apprehension Test|Bony apprehension test]]:<ref name="bushnell1">Bushnell B, Creighton R, Herring M. T[https://www.sciencedirect.com/science/article/pii/S0749806308005884 he bony apprehension test for instability of the shoulder: a prospective pilot analysis.] Arthroscopy 2008:24(9):974-82.</ref> | ||
** Positive test: Pain/reflex muscle contraction (in case of sublaxation)<ref name="bushnell1" /> | ** Positive test: Pain/reflex muscle contraction (in case of sublaxation)<ref name="bushnell1" /> | ||
{{#ev:youtube| | {{#ev:youtube|xzOlo5c7DpU}} | ||
* [http://www.physio-pedia.com/Jobes_Relocation_Test | * [http://www.physio-pedia.com/Jobes_Relocation_Test Jobe relocation test]: | ||
** Positive test: Apprehension | ** Positive test: Apprehension | ||
** Crepitus and catching may be felt during active and passive abduction and external rotation<ref name="provencher 2" /> | ** Crepitus and catching may be felt during active and passive abduction and external rotation<ref name="provencher 2" /> | ||
** Possible lesion indicated by audible/palpable clunk in active/passive abduction and external rotation or an unstable feeling during mid-range | ** Possible lesion indicated by audible/palpable clunk in active/passive abduction and external rotation or an unstable feeling during mid-range | ||
{{#ev:youtube|watch?v= | {{#ev:youtube|watch?v=K0B1lNOVnP4}} | ||
=== Special investigations === | === Special investigations === | ||
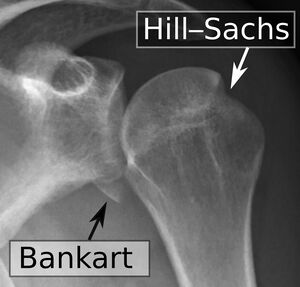
[[File:Shoulder dislocation, anteroposterior after reduction, with Bankart and Hill-Sachs lesions, with labels.jpeg|thumb|Bankart and Hill-Sachs lesions]] | |||
[[X-Rays|X-ray]]:<ref name="provencher 2" /><ref name="omoumi">Omoumi P, Teixeira P, Lecouvet F, Chung CB. [https://onlinelibrary.wiley.com/doi/pdf/10.1002/jmri.22343 Glenohumeral joint instability.] Journal of Magnetic Resonance Imaging 2011;33(1):2-16.</ref> | |||
* Grashey view (AP) in internal and external rotation; transcapular view (X-ray beam caudally from standard AP view); axillary views with exaggerated external rotation and West Pont views (if pain allows) | |||
* Important first step at effectively evaluating the glenohumeral relationship as well as osseous pathology of the humerus and the glenoid | |||
* Can detect bony lesions related to shoulder instability in the acute phase | |||
* Difficult to see Hill-Sachs lesion | |||
[[Ultrasound Scans|Ultrasound]]:<ref name="omoumi" /><ref name="kodali">Kodali P, Jones MH, Polster J, Miniaci A, Fening SD. [https://www.sciencedirect.com/science/article/pii/S1058274611000437 Accuracy of measurement of Hill-Sachs lesions with computed tomography.] Journal of shoulder and elbow surgery 2011;20(8):1328-34.</ref> | |||
* Detect and localize a compression fracture | |||
* Cost-effective, minimal exposure to excessive radiation, comfortable for patient | |||
* Hill-Sachs lesions: Apparent triangular depression in the contour of the humerus<ref name="castro" /> | |||
[[CT Scans|CT scan]]: Reliably assess the location and depth of the humeral lesion<ref name="pancione">Pancione L, Gatti G, Mecozzi B. [https://www.tandfonline.com/doi/pdf/10.1080/02841859709174380 Diagnosis of Hill-Sachs lesion of the shoulder: comparison between ultrasonography and arthro-CT.] Acta Radiologica 1997;38(4):523-6.</ref> | |||
[[MRI Scans|MRI]]: Detect pathology of the soft tissue; determine the amount of humeral and glenoid bone loss<ref name="pancione" /><ref name="pavic">Pavic R, Margetic P, Bensic M, Brnadic RL. [https://www.sciencedirect.com/science/article/pii/S0020138313701943 Diagnostic value of US, MR and MR arthrography in shoulder instability.] Injury 2013;44:S26-32.</ref> | |||
<ref name="fuller" /><ref name="cluett" /><ref name="ahmed" /> | |||
=== Outcome Measures === | |||
*[https://www.physio-pedia.com/DASH_Outcome_Measure Disabilities of the arm, shoulder and hand (DASH)] | |||
*[[Shoulder Pain and Disability Index (SPADI)]] | |||
*[https://www.physio-pedia.com/Numeric_Pain_Rating_Scale Numeric Pain Rating Scale (NPRS)] | |||
== Medical management == | == Medical management == | ||
The bony defect usually does not require treatment, though the linked glenohumeral instability and possible anterior labral injuries often need surgical repair. | |||
# Minimum glenoid bone loss and without significant involvement of the humeral head (<20%), surgical management is not indicated<ref name="andrew" />. This instability can be managed conservatively in a master sling for immobilization for 2-6 weeks, before starting with rehabilitation.<ref name="cetik" /><ref name="andrew" /> | |||
# Large Defects: Management of the bony defect (as in Hill-Sachs lesion) can be treated with bone grafting or placement of soft tissue within the defect.<ref name=":2" /> | |||
=== Surgical management === | |||
The critical size of the glenoid bone loss has been clarified as 25% of the glenoid width both biomechanically and clinically. This is the determinant factor influencing the choice of the surgical technique: soft tissue procedure or bone block procedure. <ref name=":1">Yamamoto N, Shinagawa K, Hatta T, Itoi E. Peripheral-track and central-track Hill-Sachs lesions: a new concept of assessing an on-track lesion. The American Journal of Sports Medicine. 2020 Jan;48(1):33-8.</ref> | |||
'''Arthroscopic technique''' | |||
* Remplissage procedure: Defect is filled with soft tissue, usually from the infraspinatus tendon | |||
* Second arthroplasty method: Percutaneous humeroplasty | |||
* | ** Lesion is filled by using a bone tamp brought into a drilled osseous window 180° from the lesion | ||
** Advantage: Rotational osteotomy of the humeral head is not needed and the humeral head can be restored without transpositioning the soft tissue | |||
** Limitations: Limited to moderate-sized defects; lack of management of osteochondral defects | |||
* Other procedures: Techniques that use various small bone plugs | |||
<ref name="provencher 2" /> | |||
[[File:Latarjet-Procedure, Bankart repair.jpeg|thumb|Latarjet-Procedure]] | |||
'''Open technique''' | |||
* Laterjet procedure: Most frequently done<ref name="provencher 2" /><ref name="schroder">Schroder DT, Provencher MT, Mologne TS, Muldoon MP, Cox JS. [https://www.researchgate.net/profile/Matthew_Provencher/publication/7371754_The_modified_bristow_procedure_for_anterior_shoulder_instability_26-Year_outcomes_in_Naval_Academy_Midshipmen/links/0912f509b2b2743dea000000.pdf The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy midshipmen.] The American journal of sports medicine 2006;34(5):778-86.</ref><ref name="hovellus">Hovelius L, Sandström B, Sundgren K, Saebö M. [https://www.sciencedirect.com/science/article/pii/S1058274604000916 One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I—clinical results.] Journal of shoulder and elbow surgery 2004;13(5):509-16.</ref> | |||
** Most commonly, bone from the coracoid process is used as an augment to the antero-inferior glenoid bone loss. By reforming the concavity and width of the glenoid, a Hill-Sachs lesion does not influence the anterior glenoid rim of unstable shoulders. | |||
** Successful in preventing instability over time | |||
** Negative consequences associated with the Laterjet are shoulder arthrosis and loss of function | |||
* | * Autologous bone plugs | ||
* Size-matched osteo-articular allografts | |||
* Rotational humeral osteotomy: | |||
** Osteotomy of the surgical neck to rotate the humeral head for 25° | |||
** Currently not method of choice, given the related risks and the success rates of more recent procedures. | |||
* The osseus humeral allograft bone plug technique: | |||
** A size-matched humeral bone plug of a donor is used | |||
** Approach: Delto-pectoral or deltoid-splitting | |||
** Advantages: Minimal exposure; humeral head remains in the capsule. | |||
** Disadvantage: Limited to small and moderate lesions; risks of using cadaveric tissue<ref name="provencher 2" /> | |||
== Physiotherapy management == | |||
'''Aim''': Prevent reoccurrence of dislocations | |||
The non-operative rehabilitation of the unstable shoulder consists about seven key factors. It is important to consider this in the [http://www.physio-pedia.com/Rehabilitation_program_of_the_shoulder rehabilitation program of the shoulder] after a Hill-Sachs lesion.<ref name="wilk">Wilk KE, Macrina LC, Reinold MM. Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability. North American journal of sports physical therapy 2006;1(1):16.</ref> | |||
* The onset of pathology | |||
* The degree of instability | |||
* The frequency of dislocation | |||
* The direction of instability | |||
* The onset of pathology | * Concomitant pathologies | ||
* The degree of instability | |||
* The frequency of dislocation | |||
* | |||
* Concomitant pathologies | |||
* Neuromuscular control | * Neuromuscular control | ||
* Activity level | * Activity level | ||
[[File:Stiff Brace for after Shoulder Surgery.jpeg|thumb|Stiff sling]] | |||
Physiotherapy interventions include: | |||
* 2-6 weeks of immobilization in a mastersling: | |||
** Scapula stabilization exercises | |||
** Hand, wrist and elbow exercises | |||
** Teach patient on functional adaptions (e.g. personal hygiene, dressing and undressing) | |||
** No driving while still in sling | |||
* When use of sling is discontinued (on recommendation of orthopaedic surgeon): | |||
== | ** Pendulum exercises | ||
** Passive, active-assisted and active range of motion exercises (progressions) | |||
** Abduction and external rotation is restricted during the initial phase of the rehabilitation | |||
*** Ligaments healing needs to take place to prevent dislocation | |||
** Strengthening of the deltoid, rotator cuff and periscapular (e.g. pectoralis major) muscles | |||
<ref name="andrew">Chen AL, Bosco III JA. [http://go.galegroup.com/ps/anonymous?id=GALE%7CA166094301&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=19369719&p=AONE&sw=w Glenohumeral bone loss and anterior instability.] Bulletin of the NYU hospital for joint diseases 2006 Dec 22;64(3-4):130.</ref> | |||
Post-surgical rehabilitation should be guided by the orthopaedic surgeon, and depends on the procedure that was done. | |||
- | |||
== Clinical bottom line == | == Clinical bottom line == | ||
A Hill Sachs lesion is an injury that | A Hill-Sachs lesion is an injury that occurs secondary to an anterior [http://www.physio-pedia.com/Shoulder_Dislocation shoulder dislocation]. The humeral head ‘collides’ with the anterior part of the glenoid, causing a lesion, bone loss, defect and deformity of the humeral head. This may cause a change loss of range of motion, feelings of instability and pain. A grading system is used based on the amount of bone loss or severity of the humeral head deformity. The incidence of Hill-Sachs lesion in patients with anterior shoulder instability can be as high as 100%.<ref name="provencher" /><span style="line-height: 1.5em;"><ref name="calandra" /></span> A<span style="line-height: 1.5em;">nother pathology secondary to an [http://www.physio-pedia.com/Anterior_Shoulder_Instability anterior shoulder dislocation] is a [http://www.physio-pedia.com/Bankart_lesion Bankart lesion]. This is an injury of the anterior glenoid labrum of the shoulder and often often accompanied by a Hill-Sachs lesion.<ref name="widjadja" /></span> | ||
<span style="line-height: 1.5em;">Conservative treatment is only recommended in cases of small bony defects (<20% Hill-Sachs lesion), in other cases (larger and more significant lesions), surgical treatment is needed. The conservative treatment should be based on strengthening the deltoid, the rotator cuff muscles and scapular stabilizers.<ref name="provencher" /><ref name="andrew" /></span> | |||
<span style="line-height: 1.5em;">Conservative treatment is only recommended in cases of small bony defects ( | |||
== References == | == References == | ||
| Line 205: | Line 161: | ||
<br> | <br> | ||
[[Category:Vrije_Universiteit_Brussel_Project]] | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Primary Contact]] | [[Category:Primary Contact]] | ||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Conditions]] | |||
[[Category:Shoulder - Conditions]] | |||
Latest revision as of 16:37, 25 December 2023
Original Editors - Lien Hennebel as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Jelle Van Hemelryck, Lien Hennebel, Leana Louw, Pauline Bouten, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Lucinda hampton, Shreya Pavaskar, Admin, Kim Jackson, Rachael Lowe, Fasuba Ayobami, Wanda van Niekerk, Nupur Smit Shah, 127.0.0.1 and Claire Knott
Description[edit | edit source]
A Hill-Sachs lesion is an osseous defect or "dent" of the postero-supero-lateral humeral head that occurs in association with anterior instability or dislocation of the glenohumeral joint.[1][2] It is often associated with a Bankart lesion of the glenoid.[3] This lesion is caused by an anterior shoulder dislocation which causes a humeral head impression fracture. The posterolateral aspect of the humeral head impacts on the anterior glenoid in the dislocated position, causing shoulder instability.[4][5][6]
Watch this animated description of Hill-Sachs and Bankart Lesions that can occur with a shoulder dislocation and contribute to further shoulder instability (2 minutes)
Epidemiology[edit | edit source]
The incidence of Hill-Sachs lesions are approximately 40%-90% of all anterior shoulder instability cases, and even as high as 100% in patients with recurrent anterior instability.[1] A study looking at this found Hill-Sachs lesions in 65% of acute dislocations and 93% in patients with recurrent instability.[8]
A Hill-Sachs lesion occurs in about 50% of the first-time shoulder dislocations. For people with a shoulder dislocations history (i.e. shoulder instability) humeral head compression fractures are present in most cases.[9]
Etiology[edit | edit source]
- Anterior shoulder instability:
- Approximately 47% of the lesions are associated with the initial shoulder instability according to research studies[10]
- Bankart lesion[11]
- 2.5 times more likely to for someone with either of those lesions to have the other as well[12]
- Anterior glenoid bone loss (in cases of recurrent instability)[13]
Classification[edit | edit source]
Classification systems are used to describe the amount of damage to the anterior capsule and the labrum, reflected by the depth of the lesion. Higher grade lesions are associated with increased risk of recurrent dislocation.[1][2][10]
- Grade 1: Defect in the articular surface down to (but not including) the subchondral bone
- Grade 2: Lesion includes the subchondral bone
- Grade 3: Lesion causes large defect in the subchondral bone.
Further classification can be done by looking at the percentage of the defect of humeral head involvement in the compression fracture.[14] The size of the lesion correlates in most cases to the number of previous dislocations.[15]
- Minor: <20%
- Moderate: 20%-45%
- Severe: >45%
Another classification - ON track or OFF track[16]
If the Hill-Sachs lesion engages, it is called an “off-track” Hill-Sachs lesion; if it does not engage, it is an “on-track” lesion.
Clinical Presentation[edit | edit source]
Shoulder dislocation rarely occur isolated. It causes damage to different tissues surrounding the glenohumeral joint, such as ligaments, rotator cuff tendons, joint capsule as well as the bone and cartilage of the humeral head. This occurs when the round humeral head is forcibly impacted on the edge of the glenoid, which causes compression fractures in the humeral head. This forms a dimple structure on the articular surface of the humerus - a Hill-Sachs lesion.[17][18][9]This is always caused by dislocation, not only subluxation.[17]
According to the page on shoulder dislocations, the following indicates an acute anterior glenohumeral dislocation:
- Arm held in abduction and external rotation
- Loss of normal contour of the deltoid and acromion prominent posteriorly and laterally
- Humeral head palpable anteriorly
- All movements limited and painful
- Coracoid process: Palpable fullness and positioned towards the axilla
Differential diagnosis[edit | edit source]
- Bankart lesion: Also as a result of shoulder dislocation, and often goes together[9][18]
- Pseudo-Hill-Sachs lesion: It is normal that below the level of the coracoid, the humeral head normally flattens out, and should not be mistaken as a Hill-Sachs lesion[18]
- Humeral avulsion fractures[15]
- Mid capsular tears[15]
- Floating anterior capsule[15]
- Reverse Hill-Sachs lesion: Lesion on the anterior-superior aspect of the humeral head as the result of a posterior shoulder dislocation[9][15][18]
Diagnostic Procedures[edit | edit source]
Physical examination[edit | edit source]
- Bony apprehension test:[19]
- Positive test: Pain/reflex muscle contraction (in case of sublaxation)[19]
- Jobe relocation test:
- Positive test: Apprehension
- Crepitus and catching may be felt during active and passive abduction and external rotation[4]
- Possible lesion indicated by audible/palpable clunk in active/passive abduction and external rotation or an unstable feeling during mid-range
Special investigations[edit | edit source]
- Grashey view (AP) in internal and external rotation; transcapular view (X-ray beam caudally from standard AP view); axillary views with exaggerated external rotation and West Pont views (if pain allows)
- Important first step at effectively evaluating the glenohumeral relationship as well as osseous pathology of the humerus and the glenoid
- Can detect bony lesions related to shoulder instability in the acute phase
- Difficult to see Hill-Sachs lesion
- Detect and localize a compression fracture
- Cost-effective, minimal exposure to excessive radiation, comfortable for patient
- Hill-Sachs lesions: Apparent triangular depression in the contour of the humerus[5]
CT scan: Reliably assess the location and depth of the humeral lesion[22]
MRI: Detect pathology of the soft tissue; determine the amount of humeral and glenoid bone loss[22][23]
Outcome Measures[edit | edit source]
- Disabilities of the arm, shoulder and hand (DASH)
- Shoulder Pain and Disability Index (SPADI)
- Numeric Pain Rating Scale (NPRS)
Medical management[edit | edit source]
The bony defect usually does not require treatment, though the linked glenohumeral instability and possible anterior labral injuries often need surgical repair.
- Minimum glenoid bone loss and without significant involvement of the humeral head (<20%), surgical management is not indicated[24]. This instability can be managed conservatively in a master sling for immobilization for 2-6 weeks, before starting with rehabilitation.[14][24]
- Large Defects: Management of the bony defect (as in Hill-Sachs lesion) can be treated with bone grafting or placement of soft tissue within the defect.[3]
Surgical management[edit | edit source]
The critical size of the glenoid bone loss has been clarified as 25% of the glenoid width both biomechanically and clinically. This is the determinant factor influencing the choice of the surgical technique: soft tissue procedure or bone block procedure. [25]
Arthroscopic technique
- Remplissage procedure: Defect is filled with soft tissue, usually from the infraspinatus tendon
- Second arthroplasty method: Percutaneous humeroplasty
- Lesion is filled by using a bone tamp brought into a drilled osseous window 180° from the lesion
- Advantage: Rotational osteotomy of the humeral head is not needed and the humeral head can be restored without transpositioning the soft tissue
- Limitations: Limited to moderate-sized defects; lack of management of osteochondral defects
- Other procedures: Techniques that use various small bone plugs
Open technique
- Laterjet procedure: Most frequently done[4][26][27]
- Most commonly, bone from the coracoid process is used as an augment to the antero-inferior glenoid bone loss. By reforming the concavity and width of the glenoid, a Hill-Sachs lesion does not influence the anterior glenoid rim of unstable shoulders.
- Successful in preventing instability over time
- Negative consequences associated with the Laterjet are shoulder arthrosis and loss of function
- Autologous bone plugs
- Size-matched osteo-articular allografts
- Rotational humeral osteotomy:
- Osteotomy of the surgical neck to rotate the humeral head for 25°
- Currently not method of choice, given the related risks and the success rates of more recent procedures.
- The osseus humeral allograft bone plug technique:
- A size-matched humeral bone plug of a donor is used
- Approach: Delto-pectoral or deltoid-splitting
- Advantages: Minimal exposure; humeral head remains in the capsule.
- Disadvantage: Limited to small and moderate lesions; risks of using cadaveric tissue[4]
Physiotherapy management[edit | edit source]
Aim: Prevent reoccurrence of dislocations
The non-operative rehabilitation of the unstable shoulder consists about seven key factors. It is important to consider this in the rehabilitation program of the shoulder after a Hill-Sachs lesion.[28]
- The onset of pathology
- The degree of instability
- The frequency of dislocation
- The direction of instability
- Concomitant pathologies
- Neuromuscular control
- Activity level
Physiotherapy interventions include:
- 2-6 weeks of immobilization in a mastersling:
- Scapula stabilization exercises
- Hand, wrist and elbow exercises
- Teach patient on functional adaptions (e.g. personal hygiene, dressing and undressing)
- No driving while still in sling
- When use of sling is discontinued (on recommendation of orthopaedic surgeon):
- Pendulum exercises
- Passive, active-assisted and active range of motion exercises (progressions)
- Abduction and external rotation is restricted during the initial phase of the rehabilitation
- Ligaments healing needs to take place to prevent dislocation
- Strengthening of the deltoid, rotator cuff and periscapular (e.g. pectoralis major) muscles
Post-surgical rehabilitation should be guided by the orthopaedic surgeon, and depends on the procedure that was done.
Clinical bottom line[edit | edit source]
A Hill-Sachs lesion is an injury that occurs secondary to an anterior shoulder dislocation. The humeral head ‘collides’ with the anterior part of the glenoid, causing a lesion, bone loss, defect and deformity of the humeral head. This may cause a change loss of range of motion, feelings of instability and pain. A grading system is used based on the amount of bone loss or severity of the humeral head deformity. The incidence of Hill-Sachs lesion in patients with anterior shoulder instability can be as high as 100%.[1][10] Another pathology secondary to an anterior shoulder dislocation is a Bankart lesion. This is an injury of the anterior glenoid labrum of the shoulder and often often accompanied by a Hill-Sachs lesion.[12]
Conservative treatment is only recommended in cases of small bony defects (<20% Hill-Sachs lesion), in other cases (larger and more significant lesions), surgical treatment is needed. The conservative treatment should be based on strengthening the deltoid, the rotator cuff muscles and scapular stabilizers.[1][24]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Provencher MT, Frank RM, LeClere LE, Metzger PD, Ryu JJ, Bernhardson A, Romeo AA. The Hill-Sachs lesion: diagnosis, classification, and management. Journal of the American Academy of Orthopaedic Surgeons 2012;20(4):242-52.
- ↑ 2.0 2.1 Shoulder Doc. Hill-Sachs Lesion. Available from: https://www.shoulderdoc.co.uk/article/1470 (accessed 24 December 2023).
- ↑ 3.0 3.1 Radiopedia Hills Sachs defect Available from:https://radiopaedia.org/articles/hill-sachs-defect?lang=gb (accessed 24 December 2023)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Provencher MT, Frank RM, Leclere LE, Metzger PD, Ryu JJ, Bernhardson A, Romeo AA. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012 Apr;20(4):242-52. doi: 10.5435/JAAOS-20-04-242.
- ↑ 5.0 5.1 Castro WHM, Jerosch J, Grossman TV. Examination and diagnosis of musculoskeletal disorders. Georg Thieme Verlag: Germany, 2001.
- ↑ Dodson CC, Cordasco FA. Anterior glenohumeral joint dislocations. Orthopedic Clinics of North America 2008;39(4):507-18.
- ↑ ORTHOfilms. Bankart and Hill-Sachs Lesions. Available from: https://www.youtube.com/watch?v=a6BWiufgmsc [last accessed 10.1.2023]
- ↑ Yiannakopoulos CK, Mataragas E, Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2007;23(9):985-90.
- ↑ 9.0 9.1 9.2 9.3 9.4 Wiki Radiography. Hill-Sachs and Bankart lesion. Available from:http://www.wikiradiography.net/page/Hill-Sachs+and+Bankart+Lesions (accessed 25 December 2023).
- ↑ 10.0 10.1 10.2 Calandra JJ, Baker CL, Uribe J. The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. Arthroscopy: The Journal of Arthroscopic & Related Surgery 1989;5(4):254-7.
- ↑ Horst K, Von Harten R, Weber C, Andruszkow H, Pfeifer R, Dienstknecht T, et al. Assessment of coincidence and defect sizes in Bankart and Hill–Sachs lesions after anterior shoulder dislocation: a radiological study. The British journal of radiology 2014;87(1034):20130673.
- ↑ 12.0 12.1 Widjaja AB, Tran A, Bailey M, Proper S. Correlation between Bankart and Hill‐Sachs lesions in anterior shoulder dislocation. ANZ journal of surgery 2006;76(6):436-8.
- ↑ Kim DS, Yoon YS, Yi CH. Prevalence comparison of accompanying lesions between primary and recurrent anterior dislocation in the shoulder. The American journal of sports medicine 2010;38(10):2071-6.
- ↑ 14.0 14.1 Cetik O, Uslu M, Ozsar BK. The relationship between Hill-Sachs lesion and recurrent anterior shoulder dislocation. Acta orthopaedica belgica 2007;73(2):175-8.
- ↑ 15.0 15.1 15.2 15.3 15.4 Fox JA, Sanchez A, Zajac TJ, Provencher MT. Understanding the Hill-Sachs Lesion in Its Role in Patients with Recurrent Anterior Shoulder Instability. Curr Rev Musculoskelet Med. 2017 Dec;10(4):469-479. doi: 10.1007/s12178-017-9437-0.
- ↑ Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2014 Jan 1;30(1):90-8.
- ↑ 17.0 17.1 17.2 Cluett J. Hill-Sachs Injury: Damage to the shoulder joint as result of dislocation. Orthopedics, 2013.
- ↑ 18.0 18.1 18.2 18.3 18.4 Radiopedia. Hill-Sachs lesion. https://radiopaedia.org/articles/hill-sachs-lesion (accessed 27/08/2018).
- ↑ 19.0 19.1 Bushnell B, Creighton R, Herring M. The bony apprehension test for instability of the shoulder: a prospective pilot analysis. Arthroscopy 2008:24(9):974-82.
- ↑ 20.0 20.1 Omoumi P, Teixeira P, Lecouvet F, Chung CB. Glenohumeral joint instability. Journal of Magnetic Resonance Imaging 2011;33(1):2-16.
- ↑ Kodali P, Jones MH, Polster J, Miniaci A, Fening SD. Accuracy of measurement of Hill-Sachs lesions with computed tomography. Journal of shoulder and elbow surgery 2011;20(8):1328-34.
- ↑ 22.0 22.1 Pancione L, Gatti G, Mecozzi B. Diagnosis of Hill-Sachs lesion of the shoulder: comparison between ultrasonography and arthro-CT. Acta Radiologica 1997;38(4):523-6.
- ↑ Pavic R, Margetic P, Bensic M, Brnadic RL. Diagnostic value of US, MR and MR arthrography in shoulder instability. Injury 2013;44:S26-32.
- ↑ 24.0 24.1 24.2 24.3 Chen AL, Bosco III JA. Glenohumeral bone loss and anterior instability. Bulletin of the NYU hospital for joint diseases 2006 Dec 22;64(3-4):130.
- ↑ Yamamoto N, Shinagawa K, Hatta T, Itoi E. Peripheral-track and central-track Hill-Sachs lesions: a new concept of assessing an on-track lesion. The American Journal of Sports Medicine. 2020 Jan;48(1):33-8.
- ↑ Schroder DT, Provencher MT, Mologne TS, Muldoon MP, Cox JS. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy midshipmen. The American journal of sports medicine 2006;34(5):778-86.
- ↑ Hovelius L, Sandström B, Sundgren K, Saebö M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I—clinical results. Journal of shoulder and elbow surgery 2004;13(5):509-16.
- ↑ Wilk KE, Macrina LC, Reinold MM. Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability. North American journal of sports physical therapy 2006;1(1):16.