Multiligament Injured Knee Dislocation: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Medial meniscus" to "[[Medial Meniscus") |
||
| (37 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
< | '''<br>'''<div class="editorbox"> | ||
'''Original Editors ''' - [[User:Caro De Koninck|Caro De Koninck]] | '''Original Editors ''' - [[User:Caro De Koninck|Caro De Koninck]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
A knee dislocation | A multi-ligament injured knee is commonly misnamed ''knee dislocation'' in medical literature. A dislocation causes complete joint disruption, resulting in the loss of contact of the articular surfaces.<ref name=":1" /><ref name=":2" /> Subluxation occurs when the articular surfaces stay in contact.<ref name=":1">Brautigan B, Johnson DL. [https://www.sciencedirect.com/science/article/pii/S0278591905702131 The epidemiology of knee dislocations]. Clinics in sports medicine 2000;19(3):387-97.</ref> Both of these fall under the term "multi-ligament injured knee". A multi-ligament injured knee is caused by injury of at least two out of the 4 major knee ligaments (namely [[Anterior Cruciate Ligament (ACL) Reconstruction|ACL]], PCL, [[Lateral Collateral Ligament|LCL]] and [[Medial Collateral Ligament of the Knee|MCL]]), normally associated with considerable ligamentous disruption.<ref name=":1" /><ref name="p1">Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. [https://www.sciencedirect.com/science/article/pii/S0020138310007552 Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee]. Injury 2011;42(11):1198-204.</ref><ref name=":3">Robertson A, Nutton RW, Keating JF. [https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620x.88b6.17448 Dislocation of the knee.] The Journal of bone and joint surgery 2006;88(6):706-11.</ref> It causes disruption of the active and passive stabilizers of the knee joint and is often linked with compromise to neurovascular structures and can potentially be limb theatening.<ref name=":2">Fanelli GC, editor. [https://books.google.co.za/books?hl=en&lr=&id=P-mC34cvBmwC&oi=fnd&pg=PR7&dq=The+multiple+ligament+injured+knee:+A+practical+guide+to+management.&ots=HpctQdSSWa&sig=GO7_F3ZwRx53puYdTbMDSiQnnkw#v=onepage&q=The%20multiple%20ligament%20injured%20knee%3A%20A%20practical%20guide%20to%20management.&f=false The multiple ligament injured knee: A practical guide to management.] New York: Springer Science, 2004.</ref> | ||
{{#ev:youtube|G9MPgxiZnoc}} | |||
== Clinically relevant anatomy == | |||
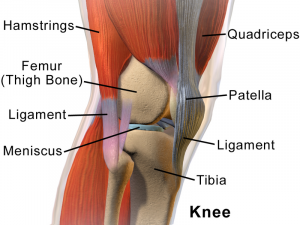
The [[Knee|knee joint]] is made up of articulations of the [[Femur|distal femur]], [[Tibia|proximal tibia]] and [[patella]].<ref name=":2" /> | |||
[[File:Knee Anatomy Side View.png|thumb|center]] | |||
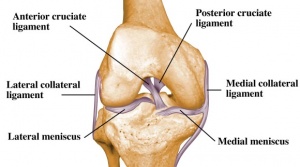
= | '''Ligaments:'''<ref name=":2" /> | ||
* [[Anterior Cruciate Ligament|ACL]] | |||
* PCL | |||
* [[Lateral Collateral Ligament|LCL]] | |||
* [[Medial Collateral Ligament of the Knee|MCL]] | |||
[[File:Ligaments-of-the-knee.jpg|thumb|300x300px|center]] | |||
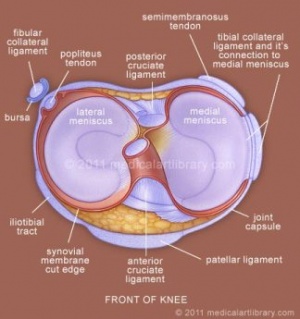
'''Menisci:'''<ref name=":2" /> | |||
* [[Medial Meniscus]] | |||
* [[Lateral meniscus]] | |||
[[File:Knee-joint-meniscus.jpg|thumb|center]] | |||
= | '''Muscles:'''<ref name=":2" /> | ||
* Anterior: | |||
** Quadriceps | |||
* Lateral: | |||
** Iliotibial band | |||
** Biceps femoris | |||
** Popliteus | |||
* Medial: | |||
** Pes anserinus ([[sartorius]], [[gracilis]], [[semitendinosus]]) | |||
** [[Semimembranosus]] | |||
* Posterior: | |||
** [[Gastrocnemius]] | |||
** [[Plantaris]] | |||
'''Vasculature:'''<ref name=":2" /> | |||
* Femoral artery | |||
* Popliteal artery | |||
'''Innervation:'''<ref name=":2" /> | |||
* Terminal branches of the following nerves: | |||
** Tibial | |||
** [[Femoral Nerve|Femoral]] | |||
** [[Sciatic Nerve|Sciatic]] - medial & lateral popliteal, common peroneal | |||
* Cutaneous nerves: | |||
** Posterior & lateral femoral cutaneous | |||
** Lateral [[Sural Nerve|sural]] cutaneous | |||
** Saphenous | |||
** Obturator | |||
=== Knee stabilizers === | |||
'''Medial''' (against valgus stress)''':'''<ref name=":2" /> | |||
* Superficial: [[Sartorius]], [[fascia]] | |||
* Middle: Posterior oblique ligament, [[semimembranosus]], [[Medial Collateral Ligament of the Knee|MCL]] | |||
* Deep: Joint capsule, medial capsular ligament | |||
'''Posteriolateral:'''<ref name=":2" /> | |||
* Superficial: Iliotibial band, [[Biceps Femoris|biceps femoris]], [[fascia]] | |||
* Middle: Patellar retinaculum, patellofemoral ligaments | |||
* Deep: [[Lateral Collateral Ligament|LCL]], [[Popliteus Muscle|popliteus tendon]], popliteofibular ligament, fabellofibular ligament, arcuate ligament, joint capsule | |||
See the page on the [[Knee|knee joint]] for in-depth information the anatomy and kinematics of the knee. This background will aid in understanding knee dislocations better. | |||
== Epidemiology/Etiology == | |||
== | Knee dislocation is estimated to be less than 0,2% of all orthopedic injuries. Complete knee dislocations are rare and usually happen after major trauma, including falls, car crashes, and other high-speed injuries.<ref name=":3" /> Spontaneous dislocation is often seen in cases associated with obesity, and make up about 20% of knee dislocations seen in practice<ref name=":2" /><ref name="p1" /> Knee dislocations can also present in congenitally and has an incidence of approximately 1 per 100,000 live births. 40-100% of these cases have additional musculoskeletal anomalies.<ref name="p3">Flint L, Meredith JW, Schwab CW. Trauma: contemporary principles and therapy. Philadelphia: Wolters Kluwer, 2008.</ref> | ||
According to a research article published in 2006, the following percentages are associated with knee dislocations:<ref name=":3" /> | |||
* | * Anterior dislocation = 40% | ||
* | * Posterior dislocation = 33% | ||
* | * Medial dislocation = 4% | ||
* | * Lateral dislocation = 18% | ||
* | * Rotary dislocation = 5% | ||
* Complete disruption of all 4 major knee stabilizing ligaments = 11% | |||
== Complications == | |||
* Vascular disruption | |||
* Iatrogenic vascular injury | |||
* Common peroneal nerve injuries | |||
* Arthrofibrosis | |||
* Compartment syndrome | |||
* Traumatic amputation | |||
* Ligament repair/reconstruction failure | |||
* Post-traumatic [[osteoarthritis]] (50% of cases) | |||
* Development of chronic pain | |||
* Long-term joint instability | |||
*Mobility limitions | |||
*Decreased quality of life | |||
<ref name=":3" /><ref name=":02" /> | |||
== Characteristics/Clinical presentation == | |||
[ | Most multi-ligament knee injuries are easily reducible with minimal assistance or even spontaneous.<ref name=":1" /> Dislocation can be suspected based on physical exam findings of joint instability/ligamentous injuries, but also based on hemarthosis and tenderness to palpation.<ref name="p4">Shearer D, Lomasney L, Pierce K. [https://europepmc.org/abstract/med/20306414 Dislocation of the knee: imaging findings]. Journal of special operations medicine: a peer reviewed journal for SOF medical professionals. 2010;10(1):43-7.</ref> It is often difficult to diagnose if a reduced knee was dislocated or subluxed without clinical witness or radiological evidence.<ref name=":1" /> Associated meniscal, osteochondral, and neurovascular injuries are often present and can complicate management.<ref name="Rihn et al.">Rihn J, Groff Y, Harner C, Cha P. [https://journals.lww.com/jaaos/Abstract/2004/09000/The_Acutely_Dislocated_Knee__Evaluation_and.8.aspx The acutely dislocated knee: evaluation and management.] J Am Acad Orthop Surg. 2004;12(5):334-46.</ref> | ||
< | '''Mechanism of injury:'''<ref name=":3" /> | ||
* Anterior dislocation: Hyperextention force | |||
* Posterior dislocation: Anterioposterior force (e.g. dashboard injury) | |||
* Medial dislocation: Varus force (often associated with tibial plateau fractures) | |||
* Lateral dislocation: Valgus force (often associated with tibial plateau fractures) | |||
* Rotary dislocation: Combination of forces | |||
< | '''Classification:'''<ref name=":3" /> | ||
* Acute: < 3 weeks post injury | |||
* Chronic: > 3 weeks post injury | |||
< | '''Associated injuries:'''<ref name=":3" /> | ||
* Popliteal artery (19%) | |||
* [[Common Peroneal Nerve|Common peroneal nerve]] (20%) | |||
* Vascular injuries (19%): | |||
** High-velocity injury (65%) | |||
** Low-velocity injury (4.8%) | |||
* [[Fracture|Fractures]] (including avulsion) - distal femur, proximal tibia (16%) | |||
* [[Compartment Syndrome|Compartment syndrome]] | |||
== Classification == | |||
Classification of knee dislocation are normally postional and/or anatomical. As most knees spontaneously reduce, postional classification can not always be used. | |||
< | The Kennedy Classification uses the position of the tibia in relation to the femur to classify knee dislocations as follows:<ref name="p1" /><ref name="p2">Henrichs A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC535529/ A review of knee dislocations.] Journal of Athletic Training 2004;39(4):365–369.</ref> | ||
*Anterior | |||
*Posterior | |||
*Lateral | |||
*Medial | |||
*Rotatory: | |||
**Anteromedial | |||
**Anterolateral | |||
**Posteromedial | |||
**Posterolateral | |||
{| border="0" cellspacing="1" cellpadding="1" | |||
|- | |||
|[[File:Lateral-knee-dislocation-1.jpg|thumb|Lateral knee dislocation]] | |||
|[[File:PosteriorKneeDisclocation.jpg|thumb|Posterior knee dislocation]] | |||
|} | |||
< | The Schenk anatomical system is based on ligament injury with additional arterial and neural injuries:<ref name=":2" /> | ||
* Type I: Single cruciate tear | |||
* Type II: Bicruciate tears without collateral tears | |||
* Type III (M): Bicruciate tears with involvement of MCL | |||
* Type III (L): LCL and posterolateral corner (PLC) tear | |||
* Type IV: All four ligaments torn | |||
* Type V: Fracture-dislocation | |||
< | ==Diagnostic procedures== | ||
It is easy to diagnose the unreduced knee, but as most cases present already reduced, it is important to do a thorough evaluation to make an accurate diagnosis and to exclude any potential associated injuries.<ref name=":3" /> Patients normally come in with a complaint of severe pain and instability, limiting activities of daily living and sport. Physical examination of a patient with a suspected knee dislocation should take place shortly after the injury is sustained.<ref name="Levy et al.2">Levy B, Peskun C, Fanelli G, Stannard J, Stuart M, MacDonald P, Marx R, Boyd J, Whelan D. [https://www.tandfonline.com/doi/abs/10.3810/psm.2010.12.1832 Diagnosis and management of knee dislocations.] Phys Sportsmed. 2010;38(4):101-11.</ref> Knee dislocation often goes hand-in-hand with concomitant injuries to other structures such as nerves and blood vessels. It is very important to do a neurovascular assessment to exclude injuries to perineal nerve and popliteal artery.<ref name=":02">Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.</ref> | |||
=== Special investigations === | |||
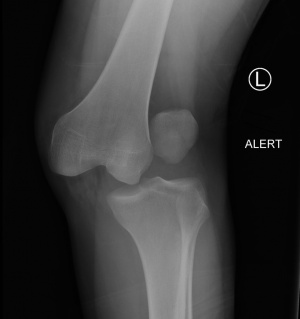
* '''[[X-Rays|X-rays]]:''' AP and lateral views should be routinely done in suspected knee dislocations due to high incidence of associated fractures | |||
* '''Doppler ultrasound:''' To assess the blood flow in the arteries | |||
* '''Ankle-brachial index:''' Can be used to determine if angiography is needed (threshold of <0.9 can positively predict a vascular injury in need of surgery) | |||
* '''Arteriography:''' Recommended if there are abnormal findings with the ankle-brachial index, as well as previous history of ischaemia or any present signs of ischaemic or circulatory compromise | |||
* '''MR angiography:''' Can be used in the acute setting as an alternative to arteriography | |||
* '''[[MRI Scans|MRI]]:''' To be used for surgical planning | |||
<ref name=":3" /><ref name="Levy et al.2" /><ref name="p12">Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. [https://www.sciencedirect.com/science/article/pii/S0020138310007552 Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee.] Injury 2011;42(11):1198-204.</ref> | |||
< | |||
< | |||
< | |||
< | |||
< | |||
== Examination == | |||
It is very important to do thorough and repeated evaluation of the neurological and vascular status for signs of injury to the common peroneal nerve, popliteal artery and to assess for compartment syndrome.<ref name=":02" /> | |||
* Observation:<ref name=":3" /> | |||
** Unreduced knee | |||
** Swelling and bruising - uncontained haemarthrosis is a major finding that can lead to the diagnosis of knee dislocation; it also suggests disruption of the joint capsule | |||
* Palpation:<ref name=":3" /><ref name=":02" /> | |||
** Diffuse pain present | |||
** Pulses - Presence of dorsalis pedis; to be used to exclude vascular injuries | |||
* Range of motion: Decreased<ref name=":3" /> | |||
* Ligament testing: This might be challenging to do in the acute, reduced knee as a result of pain and discomfort<ref name="p2" /> | |||
** PCL and posterior capsule disruption - hyperextention on passive elevation of knee | |||
** Varus and valgus laxity tested in full extention - indication of associated capsular disruption | |||
{{#ev:youtube|M0KX1rxiyqM|300}} | |||
** [[Lachman Test|Lachman test]]: Laxity present in anterior and posterior directions as a result of disruption of the cruciate ligaments | |||
{{#ev:youtube|ZvneZlW7O5s}} | |||
** [[Anterior Drawer Test of the Knee|Anterior drawer]]: Not recommended as it is challenging to perform and the reliability is compromised as a result of pain, loss of range of motion and muscle spasms | |||
** [[Pivot Shift|Pivot-shift]] and reverse pivot-shift test: Not recommended in acute cases, extremely difficult to test with swollen knee where MCL is disrupted; works well in chronic cases | |||
{| width="100%" cellspacing="1" cellpadding="1" | |||
|- | |||
|{{#ev:youtube|2TPfLOcxbTI|300}} | |||
|{{#ev:youtube|kqU55W3Y3Ho|300}} | |||
|} | |||
** [[Dial Test|Dial test]]: PCL and posterolateral corner involvement when finding of increased external rotation of the tibia is present | |||
{{#ev:youtube|BHvg9ff6yzk}} | |||
*Neural assessment:<ref name="p4" /> | |||
**Mostly done to exclude injuries to common peroneal nerve | |||
**Motor: Decreased muscle power of the ankle is a good indication of a possible injury to the common peroneal nerve | |||
**Sensory: Decreased/numbness in the presence of an injury | |||
== Outcome Measures == | |||
* [http://www.lakarhuset.com/docs/lysholmkneescoringscale.pdf Lysholm score]<ref name="p1" /> | |||
* International knee dislocation score<ref name=":3" /> | |||
* Multiligament Quality of Life questionnaire<ref name=":0">Hatch GF, Villacis D, Damodar D, Dacey M, Yi A. [https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0038-1626737 Quality of life and functional outcomes after multiligament knee reconstruction.] The journal of knee surgery 2018.</ref> | |||
* [https://www.hss.edu/secure/files/WSMC-ikdc.pdf International Knee Documentation Committee Subjective Knee Form]<ref name=":0" /> | |||
== Medical Management == | |||
Knee dislocations should be reduced as soon as possible, where after assessment of the vascular status of the leg should be done.<ref name=":3" /><ref name=":02" /> Definitive management of acute knee dislocation remains a matter of debate. Surgical reconstruction of the ligaments has proven to be more beneficial for active patients.<ref name="p1" /> Early surgical reconstruction have shown to have better outcomes when looking at knee stiffness and Lysholm scores. Conservative treatment in a range of motion brace is often chosen if the joint feels relatively stable after reduction. It is further the treatment of choice for older, more sedentary patients with the collateral ligaments still intact.<ref name="p1" /><ref name=":3" /><ref>Demirağ B, Oztürk C, Bilgen OF, Durak K. [https://europepmc.org/abstract/med/15497062 Knee dislocations: an evaluation of surgical and conservative treatment.] Turkish journal of trauma & emergency surgery 2004;10(4):239-44.</ref> | |||
=== Knee dislocation with vascular injury === | |||
* Vascular repair: | |||
** Popliteal artery bypass graft | |||
** Repair with reverse saphenous vein graft | |||
* Repair posterior capsule tear: Reattach and/or augmentation of the ligaments | |||
* Knee stabilization: | |||
** Range of motion brace (e.g. Donjoy/Exoskeleton) | |||
** Knee-spanning external fixator to protect vascular repair if instability still present | |||
* Remaining instability should be addressed at a later stage - normally only 6-12 months later | |||
<ref name=":3" /><ref name=":02" /> | |||
=== Knee dislocation without a vascular injury === | |||
* Primary repair (when swelling permits) | |||
** If not able to repair all the ligaments from the start, capsular and collateral reconstruction should be done first. Cruciate reconstruction can then be done after 6-12 weeks, when the capsule is healed. | |||
* Stabilize in a plaster of paris cast or range of motion brace (e.g. Donjoy/Exoskeleton) | |||
<ref name=":3" /><ref name=":02" /> | |||
=== Nerve injuries === | |||
There is a 20% chance of spontaneous recovery after an injury to the [[Common Peroneal Nerve|common peroneal nerve]], usually in cases where the nerve had a short distance of damage, Nerve grafting or tibialis posterior tendon transfers can be done to restore dorsiflexion.<ref name=":3" /> | |||
=== Other surgical options === | |||
'''Percutaneous quadriceps recession (PQR)'''<ref name="p1" /><ref name="p2" /> | |||
Medial and lateral incisions are made at the superior border of the patella to divide the medial and lateral quadriceps and retinaculum. The knee is then forced into flexion, while applying direct forward pressure on the femoral condyles. | |||
'''V-Y quadricepsplasty'''<ref name="p1" /><ref name="p2" /> | |||
Incision in the central part of the quadriceps tendon to allow for a V–Y advancement. The iliotibial band is released. The anterior capsule of the knee is divided transversely as far as the collateral ligaments, and the quadriceps muscle is mobilized. The knee is then reduced and flexed to 90°. The lengthened quadriceps is resutured with the knee held at 30°. This treatment has a higher morbidity compared with the PQR due to a long incision with scarring, adhesions,and wound breakdown, as well as blood loss. However, V-Y quadricepsplasty is more successful in attaining and prolonging reduction in severe and resistant cases. | |||
'''Manipulation under anaesthetics/Arthrolysis''' | |||
= | To be done in cases where stiffness persists despite therapeutic input after surgical correction of the dislocated knee. This is normally done between 3 and 6 months after initial surgery.<ref name=":3" /> | ||
=== Congenital knee dislocations === | |||
Patients who are diagnosed with knee dislocation at birth are examined within 24 hours. Early conservative management is recommended, consisting of direct reduction under gentle, persistent manual traction.<ref>Cheng C, Ko J. [https://pdfs.semanticscholar.org/4755/c63aacf571716476dd0d5c423d0fb2aa4b29.pdf Early reduction for congenital dislocation of the knee within twenty-four hours of birth]. Chang Gung Med J 2010;33:266-73. </ref> | |||
== Physiotherapy management == | |||
= | Treatment depends on the amount of damage to the different structures. Each patient will have a different treatment depending on the current stability of the patient, and eventually the other associated injuries. The goal of physiotherapy is to restore stability and regain pain-free functional mobility.<ref name="p3" /> | ||
=== Conservative management === | |||
Patients are put in a limiting range of motion brace to allow for the healing of the capsule and collateral ligaments. This will restore varus and valgus stability. During early exercises, wearing a range of motion brace is important to limit flexion to 90° and extension to 45°. After conservative treatment, rehabilitation may begin immediately.<ref name=":4" /><br> | |||
* 6 to 8 weeks initial mobilization | |||
* Weight bearing exercises | |||
* Passive and active training of the range of motion | |||
* Muscle strengthening | |||
== | The following can be done as part of the rehabilitation process. Note that it in bulleted in order of progression. Each patient should be specifically evaluated before attempting the specific treatment modalities. | ||
* Cardiovascular conditioning: Upper and midbody exercises, along with single-leg stationary bicycling | |||
* Quadriceps strengthening: Very important to prevent patellofemoral problems during rehabilitation | |||
* Light manual-resistance exercises between 45°-90° | |||
* Biodex | |||
* [[Manual Therapy: Knee|Manual therapy]] | |||
* Leg-press machine > 8 weeks of rehabilitation. During this face, the knee needs only minimal protection. These exercises should be followed by | |||
* High-speed exercises with light resistance | |||
* [[Proprioception]] (once range of motion and muscle power has been regained) | |||
<ref name=":4">Siliski JM. [https://books.google.co.za/books?hl=en&lr=&id=wPABDUH-kO8C&oi=fnd&pg=PR5&dq=Traumatic+disorders+of+the+knee.&ots=hBrpojBNvs&sig=TBxKl_Zr0ILCuxc_2d5SulcUlcE#v=onepage&q=Traumatic%20disorders%20of%20the%20knee.&f=false Traumatic disorders of the knee.] Springer Science & Business Media; 1994.</ref> | |||
=== Post-operative rehabilitation === | |||
Surgery aims to restore the anatomical structures with sufficient strength. Passive and active of the assisted range of motion rehabilitation is needed. Most patients lose range of motion and do not recover entirely after surgical intervention for a multi-ligament injured knee.<ref name=":3" /><br><br>Post-surgical rehabilitation for this injury varies according to the ligaments that were injured and repaired. An accelerated rehabilitation programme with knee bracing and early range of motion training has shown to decrease stiffness.<ref name=":3" /> Physiotherapy is not advised after PQR and V-Y quadricepsplasty.<ref name="p1" /> The following is a rough guideline, but it is important to assess each patient individually to create a customized rehabilitation programme taking their goals and expectations into account.<ref name=":3" /><ref name="p2" /> | |||
== | ==== Acute phase ==== | ||
* Mobilization: Toe-touch weight bearing in range of motion brace | |||
{{#ev:youtube|EWW-K1MyBzU}} | |||
* Continuous passive motion machine: Range of motion brace should be worn, with 40° of extension and 70° of flexion limits | |||
{{#ev:youtube|OLvJwe5GAfg}} | |||
* Isometric quadriceps exercises - very important to achieve full extension as soon as possible in the first week post-surgery | |||
** Neuromuscular facilitation techniques can be used here | |||
==== Week 7-12 ==== | |||
* Mobilization: Partial weight bearing | |||
{{#ev:youtube|lX4yoqxu3d0}} | |||
* Range of motion training can commence with the aim of achieving full range of motion: | |||
** PCL repair: Only passive and active-assisted knee flexion | |||
==== Week 13-24 ==== | |||
* Mobilization: Full weight bearing | |||
* Range of motion: Working towards full knee flexion and extension range of motion | |||
* Muscle strengthening: Closed kinetic chain exercises (start off gentle) | |||
==== Week 25-36 ==== | |||
* Muscle strengthening: Progressions | |||
* Proprioception training | |||
==== Week 37+ ==== | |||
* If able to pass functional tests: | |||
** Return to sport | |||
** Return to heavy work | |||
== | == Clinical bottom line == | ||
Multi-ligament injuries to the knee is an uncommon injury that can be easily missed as most knees relocate spontaneously or with very little effort. Knee dislocations are often associated with severe soft tissue damage, and even with advances in medical and therapeutic management, return to full baseline function is not common. Studies shown that 39% of patients classify themselves as "nearly normal", 40% as "abnormal" and 21% as "severely abnormal".<ref name=":3" /> Patients are faced with a long rehabilitation programme, with return to full activity taking at least 9 to 12 months. Most knee dislocations require reconstructive surgery. After the treatment and surgery the results are good. In most cases the damaged knees return to an almost normal state. Chronic pain is a common problem, occurring in 46% of cases. The prognosis is best with an optimal custom rehabilitation programme.<ref name=":3" /> | |||
== Resources == | |||
* [https://www.webmd.com/pain-management/knee-pain/knee-dislocation#1 What is knee dislocation?] | |||
* [https://www.orthobullets.com/trauma/1043/knee-dislocation Knee dislocation ortho bullets] | |||
== References == | == References == | ||
<references /> | <references /> | ||
<br> | |||
<br> | |||
[[Category:Vrije_Universiteit_Brussel_Project | [[Category:Injury]] | ||
[[Category:Knee_Injuries]] | |||
[[Category:Knee]] | |||
[[Category:Conditions]] [[Category:Knee - Conditions]] | |||
[[Category:Ligaments]] | |||
[[Category:Sports_Injuries]] | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Sports Medicine]] | |||
Latest revision as of 11:04, 22 January 2024
Original Editors - Caro De Koninck
Top Contributors - Estelle Hovaere, Leana Louw, Caro De Koninck, Admin, Kim Jackson, 127.0.0.1, Evan Thomas, Daphne Jackson, WikiSysop, Naomi O'Reilly and Wanda van Niekerk
Definition/Description[edit | edit source]
A multi-ligament injured knee is commonly misnamed knee dislocation in medical literature. A dislocation causes complete joint disruption, resulting in the loss of contact of the articular surfaces.[1][2] Subluxation occurs when the articular surfaces stay in contact.[1] Both of these fall under the term "multi-ligament injured knee". A multi-ligament injured knee is caused by injury of at least two out of the 4 major knee ligaments (namely ACL, PCL, LCL and MCL), normally associated with considerable ligamentous disruption.[1][3][4] It causes disruption of the active and passive stabilizers of the knee joint and is often linked with compromise to neurovascular structures and can potentially be limb theatening.[2]
Clinically relevant anatomy[edit | edit source]
The knee joint is made up of articulations of the distal femur, proximal tibia and patella.[2]
Ligaments:[2]
Menisci:[2]
Muscles:[2]
- Anterior:
- Quadriceps
- Lateral:
- Iliotibial band
- Biceps femoris
- Popliteus
- Medial:
- Pes anserinus (sartorius, gracilis, semitendinosus)
- Semimembranosus
- Posterior:
Vasculature:[2]
- Femoral artery
- Popliteal artery
Innervation:[2]
- Terminal branches of the following nerves:
- Cutaneous nerves:
- Posterior & lateral femoral cutaneous
- Lateral sural cutaneous
- Saphenous
- Obturator
Knee stabilizers[edit | edit source]
Medial (against valgus stress):[2]
- Superficial: Sartorius, fascia
- Middle: Posterior oblique ligament, semimembranosus, MCL
- Deep: Joint capsule, medial capsular ligament
Posteriolateral:[2]
- Superficial: Iliotibial band, biceps femoris, fascia
- Middle: Patellar retinaculum, patellofemoral ligaments
- Deep: LCL, popliteus tendon, popliteofibular ligament, fabellofibular ligament, arcuate ligament, joint capsule
See the page on the knee joint for in-depth information the anatomy and kinematics of the knee. This background will aid in understanding knee dislocations better.
Epidemiology/Etiology[edit | edit source]
Knee dislocation is estimated to be less than 0,2% of all orthopedic injuries. Complete knee dislocations are rare and usually happen after major trauma, including falls, car crashes, and other high-speed injuries.[4] Spontaneous dislocation is often seen in cases associated with obesity, and make up about 20% of knee dislocations seen in practice[2][3] Knee dislocations can also present in congenitally and has an incidence of approximately 1 per 100,000 live births. 40-100% of these cases have additional musculoskeletal anomalies.[5]
According to a research article published in 2006, the following percentages are associated with knee dislocations:[4]
- Anterior dislocation = 40%
- Posterior dislocation = 33%
- Medial dislocation = 4%
- Lateral dislocation = 18%
- Rotary dislocation = 5%
- Complete disruption of all 4 major knee stabilizing ligaments = 11%
Complications[edit | edit source]
- Vascular disruption
- Iatrogenic vascular injury
- Common peroneal nerve injuries
- Arthrofibrosis
- Compartment syndrome
- Traumatic amputation
- Ligament repair/reconstruction failure
- Post-traumatic osteoarthritis (50% of cases)
- Development of chronic pain
- Long-term joint instability
- Mobility limitions
- Decreased quality of life
Characteristics/Clinical presentation[edit | edit source]
Most multi-ligament knee injuries are easily reducible with minimal assistance or even spontaneous.[1] Dislocation can be suspected based on physical exam findings of joint instability/ligamentous injuries, but also based on hemarthosis and tenderness to palpation.[7] It is often difficult to diagnose if a reduced knee was dislocated or subluxed without clinical witness or radiological evidence.[1] Associated meniscal, osteochondral, and neurovascular injuries are often present and can complicate management.[8]
Mechanism of injury:[4]
- Anterior dislocation: Hyperextention force
- Posterior dislocation: Anterioposterior force (e.g. dashboard injury)
- Medial dislocation: Varus force (often associated with tibial plateau fractures)
- Lateral dislocation: Valgus force (often associated with tibial plateau fractures)
- Rotary dislocation: Combination of forces
Classification:[4]
- Acute: < 3 weeks post injury
- Chronic: > 3 weeks post injury
Associated injuries:[4]
- Popliteal artery (19%)
- Common peroneal nerve (20%)
- Vascular injuries (19%):
- High-velocity injury (65%)
- Low-velocity injury (4.8%)
- Fractures (including avulsion) - distal femur, proximal tibia (16%)
- Compartment syndrome
Classification[edit | edit source]
Classification of knee dislocation are normally postional and/or anatomical. As most knees spontaneously reduce, postional classification can not always be used.
The Kennedy Classification uses the position of the tibia in relation to the femur to classify knee dislocations as follows:[3][9]
- Anterior
- Posterior
- Lateral
- Medial
- Rotatory:
- Anteromedial
- Anterolateral
- Posteromedial
- Posterolateral
The Schenk anatomical system is based on ligament injury with additional arterial and neural injuries:[2]
- Type I: Single cruciate tear
- Type II: Bicruciate tears without collateral tears
- Type III (M): Bicruciate tears with involvement of MCL
- Type III (L): LCL and posterolateral corner (PLC) tear
- Type IV: All four ligaments torn
- Type V: Fracture-dislocation
Diagnostic procedures[edit | edit source]
It is easy to diagnose the unreduced knee, but as most cases present already reduced, it is important to do a thorough evaluation to make an accurate diagnosis and to exclude any potential associated injuries.[4] Patients normally come in with a complaint of severe pain and instability, limiting activities of daily living and sport. Physical examination of a patient with a suspected knee dislocation should take place shortly after the injury is sustained.[10] Knee dislocation often goes hand-in-hand with concomitant injuries to other structures such as nerves and blood vessels. It is very important to do a neurovascular assessment to exclude injuries to perineal nerve and popliteal artery.[6]
Special investigations[edit | edit source]
- X-rays: AP and lateral views should be routinely done in suspected knee dislocations due to high incidence of associated fractures
- Doppler ultrasound: To assess the blood flow in the arteries
- Ankle-brachial index: Can be used to determine if angiography is needed (threshold of <0.9 can positively predict a vascular injury in need of surgery)
- Arteriography: Recommended if there are abnormal findings with the ankle-brachial index, as well as previous history of ischaemia or any present signs of ischaemic or circulatory compromise
- MR angiography: Can be used in the acute setting as an alternative to arteriography
- MRI: To be used for surgical planning
Examination[edit | edit source]
It is very important to do thorough and repeated evaluation of the neurological and vascular status for signs of injury to the common peroneal nerve, popliteal artery and to assess for compartment syndrome.[6]
- Observation:[4]
- Unreduced knee
- Swelling and bruising - uncontained haemarthrosis is a major finding that can lead to the diagnosis of knee dislocation; it also suggests disruption of the joint capsule
- Palpation:[4][6]
- Diffuse pain present
- Pulses - Presence of dorsalis pedis; to be used to exclude vascular injuries
- Range of motion: Decreased[4]
- Ligament testing: This might be challenging to do in the acute, reduced knee as a result of pain and discomfort[9]
- PCL and posterior capsule disruption - hyperextention on passive elevation of knee
- Varus and valgus laxity tested in full extention - indication of associated capsular disruption
- Lachman test: Laxity present in anterior and posterior directions as a result of disruption of the cruciate ligaments
- Anterior drawer: Not recommended as it is challenging to perform and the reliability is compromised as a result of pain, loss of range of motion and muscle spasms
- Pivot-shift and reverse pivot-shift test: Not recommended in acute cases, extremely difficult to test with swollen knee where MCL is disrupted; works well in chronic cases
- Dial test: PCL and posterolateral corner involvement when finding of increased external rotation of the tibia is present
- Neural assessment:[7]
- Mostly done to exclude injuries to common peroneal nerve
- Motor: Decreased muscle power of the ankle is a good indication of a possible injury to the common peroneal nerve
- Sensory: Decreased/numbness in the presence of an injury
Outcome Measures[edit | edit source]
- Lysholm score[3]
- International knee dislocation score[4]
- Multiligament Quality of Life questionnaire[12]
- International Knee Documentation Committee Subjective Knee Form[12]
Medical Management[edit | edit source]
Knee dislocations should be reduced as soon as possible, where after assessment of the vascular status of the leg should be done.[4][6] Definitive management of acute knee dislocation remains a matter of debate. Surgical reconstruction of the ligaments has proven to be more beneficial for active patients.[3] Early surgical reconstruction have shown to have better outcomes when looking at knee stiffness and Lysholm scores. Conservative treatment in a range of motion brace is often chosen if the joint feels relatively stable after reduction. It is further the treatment of choice for older, more sedentary patients with the collateral ligaments still intact.[3][4][13]
Knee dislocation with vascular injury[edit | edit source]
- Vascular repair:
- Popliteal artery bypass graft
- Repair with reverse saphenous vein graft
- Repair posterior capsule tear: Reattach and/or augmentation of the ligaments
- Knee stabilization:
- Range of motion brace (e.g. Donjoy/Exoskeleton)
- Knee-spanning external fixator to protect vascular repair if instability still present
- Remaining instability should be addressed at a later stage - normally only 6-12 months later
Knee dislocation without a vascular injury[edit | edit source]
- Primary repair (when swelling permits)
- If not able to repair all the ligaments from the start, capsular and collateral reconstruction should be done first. Cruciate reconstruction can then be done after 6-12 weeks, when the capsule is healed.
- Stabilize in a plaster of paris cast or range of motion brace (e.g. Donjoy/Exoskeleton)
Nerve injuries[edit | edit source]
There is a 20% chance of spontaneous recovery after an injury to the common peroneal nerve, usually in cases where the nerve had a short distance of damage, Nerve grafting or tibialis posterior tendon transfers can be done to restore dorsiflexion.[4]
Other surgical options[edit | edit source]
Percutaneous quadriceps recession (PQR)[3][9]
Medial and lateral incisions are made at the superior border of the patella to divide the medial and lateral quadriceps and retinaculum. The knee is then forced into flexion, while applying direct forward pressure on the femoral condyles.
Incision in the central part of the quadriceps tendon to allow for a V–Y advancement. The iliotibial band is released. The anterior capsule of the knee is divided transversely as far as the collateral ligaments, and the quadriceps muscle is mobilized. The knee is then reduced and flexed to 90°. The lengthened quadriceps is resutured with the knee held at 30°. This treatment has a higher morbidity compared with the PQR due to a long incision with scarring, adhesions,and wound breakdown, as well as blood loss. However, V-Y quadricepsplasty is more successful in attaining and prolonging reduction in severe and resistant cases.
Manipulation under anaesthetics/Arthrolysis
To be done in cases where stiffness persists despite therapeutic input after surgical correction of the dislocated knee. This is normally done between 3 and 6 months after initial surgery.[4]
Congenital knee dislocations[edit | edit source]
Patients who are diagnosed with knee dislocation at birth are examined within 24 hours. Early conservative management is recommended, consisting of direct reduction under gentle, persistent manual traction.[14]
Physiotherapy management[edit | edit source]
Treatment depends on the amount of damage to the different structures. Each patient will have a different treatment depending on the current stability of the patient, and eventually the other associated injuries. The goal of physiotherapy is to restore stability and regain pain-free functional mobility.[5]
Conservative management[edit | edit source]
Patients are put in a limiting range of motion brace to allow for the healing of the capsule and collateral ligaments. This will restore varus and valgus stability. During early exercises, wearing a range of motion brace is important to limit flexion to 90° and extension to 45°. After conservative treatment, rehabilitation may begin immediately.[15]
- 6 to 8 weeks initial mobilization
- Weight bearing exercises
- Passive and active training of the range of motion
- Muscle strengthening
The following can be done as part of the rehabilitation process. Note that it in bulleted in order of progression. Each patient should be specifically evaluated before attempting the specific treatment modalities.
- Cardiovascular conditioning: Upper and midbody exercises, along with single-leg stationary bicycling
- Quadriceps strengthening: Very important to prevent patellofemoral problems during rehabilitation
- Light manual-resistance exercises between 45°-90°
- Biodex
- Manual therapy
- Leg-press machine > 8 weeks of rehabilitation. During this face, the knee needs only minimal protection. These exercises should be followed by
- High-speed exercises with light resistance
- Proprioception (once range of motion and muscle power has been regained)
Post-operative rehabilitation[edit | edit source]
Surgery aims to restore the anatomical structures with sufficient strength. Passive and active of the assisted range of motion rehabilitation is needed. Most patients lose range of motion and do not recover entirely after surgical intervention for a multi-ligament injured knee.[4]
Post-surgical rehabilitation for this injury varies according to the ligaments that were injured and repaired. An accelerated rehabilitation programme with knee bracing and early range of motion training has shown to decrease stiffness.[4] Physiotherapy is not advised after PQR and V-Y quadricepsplasty.[3] The following is a rough guideline, but it is important to assess each patient individually to create a customized rehabilitation programme taking their goals and expectations into account.[4][9]
Acute phase[edit | edit source]
- Mobilization: Toe-touch weight bearing in range of motion brace
- Continuous passive motion machine: Range of motion brace should be worn, with 40° of extension and 70° of flexion limits
- Isometric quadriceps exercises - very important to achieve full extension as soon as possible in the first week post-surgery
- Neuromuscular facilitation techniques can be used here
Week 7-12[edit | edit source]
- Mobilization: Partial weight bearing
- Range of motion training can commence with the aim of achieving full range of motion:
- PCL repair: Only passive and active-assisted knee flexion
Week 13-24[edit | edit source]
- Mobilization: Full weight bearing
- Range of motion: Working towards full knee flexion and extension range of motion
- Muscle strengthening: Closed kinetic chain exercises (start off gentle)
Week 25-36[edit | edit source]
- Muscle strengthening: Progressions
- Proprioception training
Week 37+[edit | edit source]
- If able to pass functional tests:
- Return to sport
- Return to heavy work
Clinical bottom line[edit | edit source]
Multi-ligament injuries to the knee is an uncommon injury that can be easily missed as most knees relocate spontaneously or with very little effort. Knee dislocations are often associated with severe soft tissue damage, and even with advances in medical and therapeutic management, return to full baseline function is not common. Studies shown that 39% of patients classify themselves as "nearly normal", 40% as "abnormal" and 21% as "severely abnormal".[4] Patients are faced with a long rehabilitation programme, with return to full activity taking at least 9 to 12 months. Most knee dislocations require reconstructive surgery. After the treatment and surgery the results are good. In most cases the damaged knees return to an almost normal state. Chronic pain is a common problem, occurring in 46% of cases. The prognosis is best with an optimal custom rehabilitation programme.[4]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Brautigan B, Johnson DL. The epidemiology of knee dislocations. Clinics in sports medicine 2000;19(3):387-97.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Fanelli GC, editor. The multiple ligament injured knee: A practical guide to management. New York: Springer Science, 2004.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee. Injury 2011;42(11):1198-204.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 Robertson A, Nutton RW, Keating JF. Dislocation of the knee. The Journal of bone and joint surgery 2006;88(6):706-11.
- ↑ 5.0 5.1 Flint L, Meredith JW, Schwab CW. Trauma: contemporary principles and therapy. Philadelphia: Wolters Kluwer, 2008.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.
- ↑ 7.0 7.1 Shearer D, Lomasney L, Pierce K. Dislocation of the knee: imaging findings. Journal of special operations medicine: a peer reviewed journal for SOF medical professionals. 2010;10(1):43-7.
- ↑ Rihn J, Groff Y, Harner C, Cha P. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12(5):334-46.
- ↑ 9.0 9.1 9.2 9.3 9.4 Henrichs A. A review of knee dislocations. Journal of Athletic Training 2004;39(4):365–369.
- ↑ 10.0 10.1 Levy B, Peskun C, Fanelli G, Stannard J, Stuart M, MacDonald P, Marx R, Boyd J, Whelan D. Diagnosis and management of knee dislocations. Phys Sportsmed. 2010;38(4):101-11.
- ↑ Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. Acute knee dislocation: An evidence based approach to the management of the multiligament injured knee. Injury 2011;42(11):1198-204.
- ↑ 12.0 12.1 Hatch GF, Villacis D, Damodar D, Dacey M, Yi A. Quality of life and functional outcomes after multiligament knee reconstruction. The journal of knee surgery 2018.
- ↑ Demirağ B, Oztürk C, Bilgen OF, Durak K. Knee dislocations: an evaluation of surgical and conservative treatment. Turkish journal of trauma & emergency surgery 2004;10(4):239-44.
- ↑ Cheng C, Ko J. Early reduction for congenital dislocation of the knee within twenty-four hours of birth. Chang Gung Med J 2010;33:266-73.
- ↑ 15.0 15.1 Siliski JM. Traumatic disorders of the knee. Springer Science & Business Media; 1994.