Paraneoplastic Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 27: | Line 27: | ||
==<u></u>Clinical Presentation == | ==<u></u>Clinical Presentation == | ||
Paraneoplastic syndrome involves multi-organ system in the body with heterogeneous and complex clinical manifestations in the setting of underlying malignancy. | |||
Clinical presentations are categorized based on the organ system as follows. | |||
# '''Nervous System''' - Signs and symptoms are based on the part of the nervous system that is affected by a paraneoplastic syndrome eg central nervous system, neuromuscular junction, or peripheral nervous system. A patient may present with seizure, cognitive dysfunction, personality change, psychosis, insomnia, ataxia, dysarthria, dysphagia, cranial nerve deficits, and sensorimotor abnormalities. | |||
* '''Central Nervous System''' eg Paraneoplastic encephalitis/encephalomyelitis; Subacute cerebellar degeneration; Opsoclonus-myoclonus syndrome | |||
* '''Neuromuscular Junction''' eg [[Myasthenia Gravis]]; [[Lambert-Eaton Myasthenic Syndrome|Lambert-Eaton]] myasthenic syndrome (LEMS) | |||
* '''Peripheral Nervous System''' eg Autonomic [[Neuropathies|neuropathy]]; Subacute sensory neuropathy | |||
'''2. Endocrine''' eg [[Cushing's Syndrome|Cushing]] syndrome; Syndrome of inappropriate antidiuretic hormone secretion (SIADH); Hypercalcemia | |||
Paraneoplastic | '''3. Rheumatological''' eg Paraneoplastic polyarthritis; [[Polymyalgia Rheumatica|Polymyalgia rheumatica]]; Multicentric reticulohistiocytosis; Hypertrophic osteoarthropathy | ||
'''4. Hematological''' Hematologic manifestations of the paraneoplastic syndrome are generally asymptomatic but can be manifested as pallor, fatigue, dyspnea, and venous thromboembolism. Hematologic syndromes are characterized by thrombocytosis, granulocytosis, eosinophilia, pure red cell aplasia, disseminated intravascular coagulation, and leukemoid reactions. | |||
'''5. Dermatological eg''' Acanthosis nigricans; Paraneoplastic pemphigus; Sweet syndrome; Leukocytoclastic vasculitis; Dermatomyositis | |||
'''6. Renal eg''' Electrolyte imbalance ([[hypokalemia]], hypo or hypernatremia, hyperphosphatemia) causing nephropathy and acid-base disturbance due to ectopic hormones produced by tumor cells such as ACTH and ADH.[14] Nephrotic syndrome can also be one of the manifestations of paraneoplastic syndrome. | |||
'''7.Miscellaneous eg''' Fever, cachexia, [[Anorexia Nervosa|anorexia]], dysgeusia<ref name=":1" /><sup></sup><sup></sup><sup></sup> | |||
< | |||
== <sup></sup>Management == | == <sup></sup>Management == | ||
* Management of the patients is based on type, severity, and location of the paraneoplastic syndrome. First, therapeutic options are to treat underlying malignancy with [[Chemotherapy Side Effects and Syndromes|chemotherapy]], [[Radiation Side Effects and Syndromes|radiation]], or surgery. | *[[File:National-cancer-institute-0YBIMOqQzt0-unsplash.jpg|right|frameless]]Management of the patients is based on type, severity, and location of the paraneoplastic syndrome. First, therapeutic options are to treat underlying malignancy with [[Chemotherapy Side Effects and Syndromes|chemotherapy]], [[Radiation Side Effects and Syndromes|radiation]], or surgery. | ||
* Other therapeutic options are immunosuppression with [[Corticosteroids in the Management of Rheumatoid Arthritis|corticosteroids]] or other immunosuppressive drugs, intravenous immunoglobulins, plasma exchange, or plasmapheresis. | * Other therapeutic options are immunosuppression with [[Corticosteroids in the Management of Rheumatoid Arthritis|corticosteroids]] or other immunosuppressive drugs, intravenous immunoglobulins, plasma exchange, or plasmapheresis. | ||
| Line 96: | Line 71: | ||
If the physicians cannot find a malignant tumor, the syndrome may be the cause of a tumor that is too small to locate. In this instance, the physician will continue to have follow-up imaging conducted every three to six months for a several years unless the cause is identified. <ref name="p1" /><sup></sup><sup></sup><sup></sup> | If the physicians cannot find a malignant tumor, the syndrome may be the cause of a tumor that is too small to locate. In this instance, the physician will continue to have follow-up imaging conducted every three to six months for a several years unless the cause is identified. <ref name="p1" /><sup></sup><sup></sup><sup></sup> | ||
== Physical Therapy Management == | == Physical Therapy Management == | ||
[[File:Breast Cancer Exercise Classes.jpg|right|frameless]] | |||
People with paraneoplastic syndrome can have difficulty with walking, [[balance]], [[Coordination Exercises|coordination]], [[muscle]] tone, sensory of where the body is in space, and vertigo. | |||
* All of these symptoms the physical therapist can treat with traditional therapy. | |||
* Precautions must be taken into account for the cancer or neoplasm that is involved.<ref name="p2" /><br> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
# Abdominal Aortic Aneurysm | # Abdominal Aortic Aneurysm | ||
| Line 117: | Line 95: | ||
# Superficial Thrombophlebitis | # Superficial Thrombophlebitis | ||
# Systemic Lupus Erythematosus | # Systemic Lupus Erythematosus | ||
# Undifferentiated Connective-Tissue Disease <sup><ref name="p4" /></sup> | # Undifferentiated Connective-Tissue Disease <sup><ref name="p4">Medscape Reference. Paraneoplastic Syndromes. http://emedicine.medscape.com/article/280744-differential. (accessed 18 March 2013).</ref></sup> | ||
== Case Reports/ Case Studies == | == Case Reports/ Case Studies == | ||
''A case of paraneoplastic syndrome accompanied by two types of cancer'': [http://jnnp.bmj.com/content/72/3/408.full.pdf+html jnnp.bmj.com/content/72/3/408.full.pdf+html] | ''A case of paraneoplastic syndrome accompanied by two types of cancer'': [http://jnnp.bmj.com/content/72/3/408.full.pdf+html jnnp.bmj.com/content/72/3/408.full.pdf+html] | ||
== Conclusion == | == Conclusion == | ||
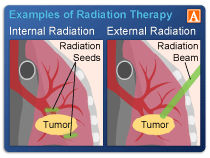
[[File:Internal-and-External-Radiation-Therapy.png|right|frameless|210x210px]] | |||
The diagnosis and management of paraneoplastic syndromes is difficult. | The diagnosis and management of paraneoplastic syndromes is difficult. | ||
* In most cases, there is an underlying malignancy responsible. | * In most cases, there is an underlying malignancy responsible. | ||
Revision as of 01:35, 15 July 2020
Original Editors - Brittany Chorley & Seth Chorley from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Seth Chorley, Brittany Chorley, Lucinda hampton, Admin, Kim Jackson, Priya Gulla, Elaine Lonnemann, Rujuta Naik, WikiSysop, 127.0.0.1, Vidya Acharya, Claire Knott, Wendy Walker, Mariam Hashem and Adam Vallely Farrell
Introduction[edit | edit source]
Paraneoplastic syndromes (PNS) are rare clinical syndromes due to the systemic effects of tumours; they are unrelated to tumour size, invasiveness or metastases. Carcinoid syndrome is a paraneoplastic syndrome comprising the signs and symptoms that occur secondary to carcinoid tumors See image R
- Recent years have seen considerable advances leading to improved understanding of their pathophysiology and increased recognition of new PNS entities and PNS associated tumours.
- Diagnosis is still frequently missed or delayed.
- Diverse organs and systems are affected by the associated tumours- which may be benign or malignant.
- PNS can occur concurrently with tumour diagnosis, before tumour is diagnosed and even after tumours have been resected[1].
- It is hypothesized that paraneoplastic syndrome occurs when cancer-fighting antibodies or white blood cells (known as T cells) mistakenly attack normal cells in the nervous system. Another hypothesis is that the neoplasm secretes hormones or cytokines that cause the symptoms to occur. Neurological symptoms can develop over a period of days to weeks and usually occur prior to the tumor being discovered. [2]
- The symptoms typically presents in the middle-aged to older population. Also, it is common in individuals with lung, ovarian, lymphatic, or breast cancer. The most common cancer associated with paraneoplastic syndrome is small cell cancer of the lungs. [3]
Etiology[edit | edit source]
PNS are largely due to two main causes:
- Those due to tumour secretions of hormones, functionally active peptides, enzymes cytokines
- Those due to tumours operating through auto-immune/immunological mechanisms with cross-reacting antibodies between neoplastic and normal tissues. Nb Remission of symptoms often follows resection of humoral secretory tumours but not always of tumours due to immunological mechanisms[1].
Epidemiology[edit | edit source]
- Precise incidence and prevalence of the paraneoplastic syndrome are unknown (due to the rarity of disease). Can occur with any malignancy.
- A review of the literature suggests that paraneoplastic syndrome occurs in up to 8% of cancer patients.
- Neurological manifestation in the form of neuropathies is common.
- Males and females are affected equally.[4]
Clinical Presentation[edit | edit source]
Paraneoplastic syndrome involves multi-organ system in the body with heterogeneous and complex clinical manifestations in the setting of underlying malignancy.
Clinical presentations are categorized based on the organ system as follows.
- Nervous System - Signs and symptoms are based on the part of the nervous system that is affected by a paraneoplastic syndrome eg central nervous system, neuromuscular junction, or peripheral nervous system. A patient may present with seizure, cognitive dysfunction, personality change, psychosis, insomnia, ataxia, dysarthria, dysphagia, cranial nerve deficits, and sensorimotor abnormalities.
- Central Nervous System eg Paraneoplastic encephalitis/encephalomyelitis; Subacute cerebellar degeneration; Opsoclonus-myoclonus syndrome
- Neuromuscular Junction eg Myasthenia Gravis; Lambert-Eaton myasthenic syndrome (LEMS)
- Peripheral Nervous System eg Autonomic neuropathy; Subacute sensory neuropathy
2. Endocrine eg Cushing syndrome; Syndrome of inappropriate antidiuretic hormone secretion (SIADH); Hypercalcemia
3. Rheumatological eg Paraneoplastic polyarthritis; Polymyalgia rheumatica; Multicentric reticulohistiocytosis; Hypertrophic osteoarthropathy
4. Hematological Hematologic manifestations of the paraneoplastic syndrome are generally asymptomatic but can be manifested as pallor, fatigue, dyspnea, and venous thromboembolism. Hematologic syndromes are characterized by thrombocytosis, granulocytosis, eosinophilia, pure red cell aplasia, disseminated intravascular coagulation, and leukemoid reactions.
5. Dermatological eg Acanthosis nigricans; Paraneoplastic pemphigus; Sweet syndrome; Leukocytoclastic vasculitis; Dermatomyositis
6. Renal eg Electrolyte imbalance (hypokalemia, hypo or hypernatremia, hyperphosphatemia) causing nephropathy and acid-base disturbance due to ectopic hormones produced by tumor cells such as ACTH and ADH.[14] Nephrotic syndrome can also be one of the manifestations of paraneoplastic syndrome.
7.Miscellaneous eg Fever, cachexia, anorexia, dysgeusia[4]
Management[edit | edit source]
- Management of the patients is based on type, severity, and location of the paraneoplastic syndrome. First, therapeutic options are to treat underlying malignancy with chemotherapy, radiation, or surgery.
- Other therapeutic options are immunosuppression with corticosteroids or other immunosuppressive drugs, intravenous immunoglobulins, plasma exchange, or plasmapheresis.
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
First, a health care provider will perform a clinical exam that would include a general physical and neurological screening. Tests that would be involved in the neurological screening could include reflexes, sensation, myotomes, balance, and coordination.
Laboratory tests that could be utilized to diagnose paraneoplastic syndrome include:
Blood tests: This may identify antibodies typically associated with paraneoplastic syndrome. However, some people who have the syndrome do not have the antibody, and some people who do not have the syndrome actually have the antibody. Blood tests can also identify an infection, disorder of nutrient processing, or hormone disorder.
Spinal tap: A neurologist or nurse will insert a needle into your lumbar spine to extract a small amount of cerebrospinal fluid (CSF). At times, paraneoplastic antibodies may be present in the CSF but not in the blood.
Imaging tests that could be utilized to diagnose paraneoplastic syndrome include:
CT Scan
MRI
PET Scan
PET-CT, which may enhance the detection rate of small cancers
If the physicians cannot find a malignant tumor, the syndrome may be the cause of a tumor that is too small to locate. In this instance, the physician will continue to have follow-up imaging conducted every three to six months for a several years unless the cause is identified. [2]
Physical Therapy Management[edit | edit source]
People with paraneoplastic syndrome can have difficulty with walking, balance, coordination, muscle tone, sensory of where the body is in space, and vertigo.
- All of these symptoms the physical therapist can treat with traditional therapy.
- Precautions must be taken into account for the cancer or neoplasm that is involved.[3]
Differential Diagnosis[edit | edit source]
- Abdominal Aortic Aneurysm
- Anemia
- Antithrombin Deficiency
- Attention Deficit Hyperactivity Disorder
- Bone Marrow Failure
- Chronic Fatigue Syndrome
- Dermatomyositis
- Diabetes Mellitus, Type 1
- Glomerulonephritis, Acute
- Mixed Connective-Tissue Disease
- Myelodysplastic Syndrome
- Nephrotic Syndrome
- Personality Disorders
- Polycythemia Vera
- Polymyalgia Rheumatica
- Scleroderma
- Superficial Thrombophlebitis
- Systemic Lupus Erythematosus
- Undifferentiated Connective-Tissue Disease [5]
Case Reports/ Case Studies[edit | edit source]
A case of paraneoplastic syndrome accompanied by two types of cancer: jnnp.bmj.com/content/72/3/408.full.pdf+html
Conclusion[edit | edit source]
The diagnosis and management of paraneoplastic syndromes is difficult.
- In most cases, there is an underlying malignancy responsible.
- Due to the numerous causes, the condition is best managed by an interprofessional team (including a pathologist, oncologist, radiologist, hematologist, nurse specialist, and an internist).
- Once the cause is discovered, it needs to be treated.
The management of the patients is based on type, severity, and location of the paraneoplastic syndrome.
- First, therapeutic options are to treat underlying malignancy with chemotherapy, radiation, or surgery.
- Other therapeutic options are immunosuppression with corticosteroids or other immunosuppressive drugs, intravenous immunoglobulins, plasma exchange, or plasmapheresis.[4]
References[edit | edit source]
- ↑ 1.0 1.1 Henry K. Paraneoplastic syndromes: definitions, classification, pathophysiology and principles of treatment. InSeminars in diagnostic pathology 2019 Jul 1 (Vol. 36, No. 4, pp. 204-210). WB Saunders.Available from:https://www.sciencedirect.com/science/article/abs/pii/S0740257019300097 (last accessed 15.7.2020)
- ↑ 2.0 2.1 Mayo Clinic. Paraneoplastic syndromes of the nervous system. http://www.mayoclinic.com/health/paraneoplastic-syndromes/DS00840. (accessed 18 March 2013).
- ↑ 3.0 3.1 National Institute of Neurological Disorders and Stroke. NINDS Paraneoplastic Syndromes Information Page. http://www.ninds.nih.gov/disorders/paraneoplastic/paraneoplastic.htm. (accessed 18 March 2013).
- ↑ 4.0 4.1 4.2 Thapa B, Ramphul K. Paraneoplastic syndromes. InStatPearls [Internet] 2020 Jun 27. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK507890/ (last accessed 15.7.2020)
- ↑ Medscape Reference. Paraneoplastic Syndromes. http://emedicine.medscape.com/article/280744-differential. (accessed 18 March 2013).