Posterior Cruciate Ligament Injury: Difference between revisions
Leana Louw (talk | contribs) No edit summary |
Leana Louw (talk | contribs) No edit summary |
||
| Line 89: | Line 89: | ||
{{#ev:youtube|7vgTMnfP4fs}} | {{#ev:youtube|7vgTMnfP4fs}} | ||
* Quadriceps active test<ref name="p1" /><ref name="p7" /> | * Quadriceps active test<ref name="p1" /><ref name="p7" /> | ||
{{#ev:youtube|tQCacgQgC-s}} | |||
* [[Dial Test|Dial test]] or tibial external rotation test | * [[Dial Test|Dial test]] or tibial external rotation test | ||
{{#ev:youtube|3UGffd71KyI}} | {{#ev:youtube|3UGffd71KyI}} | ||
Revision as of 18:08, 22 August 2018
Original Editors - Sigrid Bortels
Top Contributors - Camille Dewaele, Sigrid Bortels, Leana Louw, Mariam Hashem, Kim Jackson, Admin, Rachael Lowe, Kai A. Sigel, 127.0.0.1, Vanderpooten Willem, WikiSysop, Fasuba Ayobami, Simisola Ajeyalemi, Wanda van Niekerk, Hana Vezsenyi, Claire Knott, Jess Bell, Evan Thomas, Robin Tacchetti, Oyemi Sillo, Naomi O'Reilly and Daphne Jackson
***Editing in process - come back later for updated information***
Definition/Description[edit | edit source]
Injury to the posterior cruciate ligament (PCL) can range from a stretch to a total tear or rupture of the ligament. These injuries are less common than anterior cruciate ligament (ACL) injuries as the PCL is broader and stronger.[1]
Clinically relevant anatomy[edit | edit source]
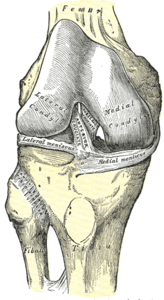
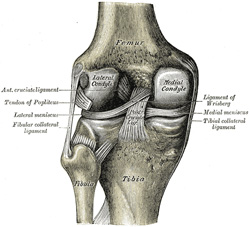
The PCL is one of the two cruciate ligaments of the knee. It acts as the major stabilizing ligament of the knee. and prevents the tibia from excessive posterior displacement in relation to the femur. It also functions to prevent hyper-extension and limits internal rotation, adduction and abduction at the knee joint.[1] The PCL is twice as thick as the ACL which results in less injuries than the ACL due to the stronger nature. As a result, PCL injuries are less common than ACL injuries.
It originates at the internal surface of the medial femoral condyle and inserts on the center of the posterior aspect of the tibial plateau, 1 cm below the articular surface of the tibia[1][2]. It crosses the ACL to form an 'X'. The PCL consists of two inseparable bundles: the wide anterolateral (AL) bundle and the smaller posteromedial (PM) bundle.[1] The AL bundle is most tight in mid-flexion and internal rotation of the knee, while the PM bundle is most tight in extension and deep flexion of the knee. The orientation of the fibers varies between bundles. The AL bundle is more horizontally orientated in extension and becomes more vertical as the knee is flexed beyond 30°. The PM bundle is vertically orientated in knee extension and becomes more horizontal through a similar range of motion.[1][2]
Epidemiology/Etiology[edit | edit source]
Epidemiology[edit | edit source]
The mean age of people with acute PCL injuries range between 20-30's. Injuries to the PCL can occur isolated, mostly as a result of sport, as well as combined (see multi-ligament knee injuries), usually caused by motor vehicle accidents.[3]
A 2% incidence is estimated for PCL injuries, and it can range from 3,5-20% for operated, isolated and combined PCL injuries.[1]
Etiology[edit | edit source]
The most frequent mechanism of injury is a direct blow to the anterior aspect of the proximal tibia on a flexed knee with the ankle in plantarflexion[3]. This often occurs as dashboard injuries (posterior force to the tibia in a flexed knee) during motor vehicle accidents and results in posterior translation of the tibia. Hyper-extension and rotational or varus/valgus stress mechanisms may also be responsible for PCL tears.[1][4][5] These injuries occurs mostly during sports such as football, soccer and skiing. Isolated PCL injuries are commonly reported in athletes, with hyper-flexion being the most frequent mechanism of injury.[4][6] Further mechanisms of PCL injury include bad landings from a jump, a simple misstep or fast direction change.[4][5]
Characteristics/Clinical presentation[edit | edit source]
Characteristics[edit | edit source]
PCL injuries present in different degrees according to the severity.
Grade 1: Limited damage with only microscopic tears in the ligament, mostly as the result of an overstretch. It is still able to function and stabilize the knee.[7]
Grade 2: The ligament is partially torn. There is a feeling of instability[7].
Grade 3: Complete ligament tear or rupture. This type of injury is mostly accompanied by a sprain of the ACL and/or collateral ligaments.[1][7]
Clinical presentation[edit | edit source]
A distinction can be made between the symptoms of an acute and chronic PCL injury[8].
Acute PCL injury[edit | edit source]
- Isolated injury:
Symptoms are often vague and minimal, with patients often not even feeling or noticing the injury.l[1][2][8] Minimal pain, swelling, instability and full range of motion is present, as well as a near-normal gait pattern.[1][2][8]
- Combination with other ligamentous injuries:
Symptoms differ according to the extent of the knee injury. This includes swelling, pain, a feeling of instability, limited range of motion and difficulty with mobilisation. Bruising may also be present.[1]
Chronic PCL injury[edit | edit source]
Patients with a chronic PCL injury are not always able to recall a mechanism of injury. Common complaints are discomfort with weight-bearing in a semi flexed position (e.g. climbing stairs or squatting) and aching in the knee when walking long distances. Complaints of instability are also often present, mostly when walking on an uneven surface[8]. Retropatellar pain and pain in the medial compartment of the knee may also be present[8]. Potential swelling and stiffness depend on the degree of associated chondral damage.[8]
Differential diagnosis[edit | edit source]
- ACL injury
- Medial collateral ligament injury
- Talofibular ligament injury
- Menisci injuries
- Patellofemoral joint injuries
- Posterolateral knee injury and associated varus instability
Uncommon:[9]
- Multiligament knee injury
- Femoral condyle fracture
- Tibial plateau fracture
Diagnostic procedures[edit | edit source]
Physical examination[edit | edit source]
- Neurovascular examination to rule out concurrent injuries[10]
- Palpation: Minimum/no swelling in isolated injury [11]
- Muscle power
- Range of motion
Special tests[edit | edit source]
- Posterior drawer: One of the most accurate tests for PCL injury and can only be executed when there is no swelling in the knee joint[1][4]
- Posterior Lachman test: A slight increase in posterior translation indicates a posterolateral ligament complex injury[2][4]
- Dial test or tibial external rotation test
- Special tests to rule out concurrent knee injuries:[1][2][4]
- Varus/Valgus stress tests
- External rotation recurvatum test
- Reverse pivot shift test
Special investigations[edit | edit source]
- X-rays:
- AP, tunnel, sunrise, stress and a lateral views (best to detect lateral sag)
- X-rays can be done in different positions, e.g. standing and weight-bearing with 45° knee flexion
- Assists in early identification of PCL avulsion fractures
- Chronic: Assess joint space narrowing (preferably including weight-bearing and sunrise views)
- MRI:
- Acute: Determine grade of injury, as well as evaluating other potentially injured structures (e.g. ligaments, meniscus and/or cartilage structures of the knee)
- Chronic: MRI may appear normal in grade I and II injures
- Bone scans: Best in chronic cases with pain and instability.
- Detect early arthritic changes before MRI or Xray. These patients have a higher risk of developing articular cartilage degenerative changes, shown by areas of increased radiotracer uptake, most commonly in the medial and patellofemoral compartments.
- Ultrasound: More cost effective than MRI for evaluation
- Arteriogram: Evaluate the vascular status in the limb
Outcome measures[edit | edit source]
- Noyes knee score Questionnaire
- International Knee Documentation Committee (IKDC)
Medical management[edit | edit source]
PCL avulsion fracture. These fractures heal well when operated early. In case of a chronic PCL injury plain radiographs can help assess the joint space narrowing, preferably including weightbearing and sunrise view.[10][6]
Acute PCL injury:
The treatment used for an acute, isolated grade I or II sprain is most commonly non-operative.[10][1] The conditions for this treatment are: a posterior drawer less than 10 mm, a decrease in posterior drawer excursion with internal rotation on the femur, less than 5° abnormal rotary laxity and/or no significant increased valgus-varus laxity.[10][5]
It is usually adequate to relatively immobilize the knee and to use crutches during a two week period for protected weightbearing. Subsequently physical therapy, which mainly includes protective quadriceps muscle rehabilitation, will be a determining factor for further rehabilitation.[10][1]
A 3rd grade injury can also be cured in a non-operative manner. Because of the high probability of injuries to other posterolateral structures, an immobilization period of two to four weeks in full extension is recommended. Because of this the posterior tibial sag is minimalized, which means that less force is applied to the damaged PCL and posterolateral structures. Subsequently physical therapy will mainly consist of quadriceps rehabilitation and straight-leg raise exercises.
If the patient is a young athlete, they will sooner decide to treat the injury operatively. Thay way the athlete will be able to reach his level again.
A grade III injury is most of the time a combined injury. In this case there will be a surgical intervention (reconstruction of the ligaments).
Chronic PCL injury:
If the patient has a chronic isolated PCL injury grade I or II, the treatment comprises physical therapy. When the patient develops recurrent pain and swelling a bone scan is recommended. The results of this treatment are controversial. Wind et al[10] recommend surgical intervention when the scan is positive and the patient is unable to modify his activities. Harner et al[1]
recommends a reduction in activities until the pain and swelling subside. They do not recommend a surgical intervention. Both articles recommend a surgical intervention in case of a grade III sprain.
A chronic PCL injury can also be a combined injury. Just as in the acute injuries surgery is indispensable.The severity of the injthe treatment protocolury determines
Non-operative treatment
Non-operative management, used in acute isolated grade I or II PCL injuries, includes protective weightbearing with crutches. The focus of the rehabilitation lies on reducing knee joint effusion, restoring knee range of motion and regaining strength, especially of the quadriceps muscle group. This is necessary because of the two week period of relative immobilization of the knee that is recommended by physicians.
Grade I and II PCL tears usually recover rapidly. Most patients are satisfied with the outcome.
In case of athletes the goal is to return to their sport activities in two to four weeks after the injury.[10][6] (level of evidence 3A)
Grade III tears can also be treated non-operatively. These patients are usually immobilized for two to four weeks in full extension, because often the PLC or posterior medial complex (PMC) is also injured. The full extension eliminates the posterior subluxation caused by the hamstrings and allows the injured soft tissue structures to heal. Patients that continue to have pain and do not progress well enough will need surgical intervention. Non-operatively manage grade III tears delay the return to sport for three to four months.[10][6]
Chronic PCL injuries can be adequately treated with physical therapy. A brace is used during this treatment. Initially the brace prevents the terminal 15° of extension. After a while the brace is opened to full extension. But Wind et al[9] do not think the brace prevents posterior tibial motion.[10]
There are contradictory opinions about the effect of a knee brace. Bracing of the PCL injured knee is directed toward improvements in dynamic knee stability and prevention of posterior tibial translation during activity. The study of Jacobi et al(1) to determine the effectiveness of bracing a PCL injured knee concluded that after wearing the brace for four months there was a decreased posterior sag after two years. However, this study failed to include a control group and therefore they could not conclude that the decrease was the result of the brace.[4] Fanelli et al[6] did not find a helpful effects of wearing braces on the rehabilitation of PCL injuries.[6]
If the patients report symptoms like pain and recurrent swelling and the Xrays show negative results, Wind et al[10] recommend a bone scan and MRI. If the bone scan has a positive result in patients with grade I or II tears, who can’t modify their activities, or patients with a grade III tear, a surgical intervention is recommended.[10][6]
Operative treatment
Surgical reconstruction of the PCL is recommended in acute injuries with severe posterior tibia subluxation and instability, if the posterior translation is greater than 10mm or if there are multiple ligamentous injuries.
If there are other ligaments damaged as well, surgery is often performed within two weeks after the injury. This gives the best anatomical ligament repair of the PCL and gives less capsular scarring. The PCL reconstruction is often not the first surgery performed. It is secondary to repairing the other injured structures, such as the PLC or PMC, because this forms less scar tissue. The PLC scars quickly, which makes anatomical repair difficult if the reconstruction is delayed for more than three weeks following injury.
The primary objective during a PCL reconstruction is to restore normal knee mechanics and dynamic knee stability.[10][6]
There are different options of the optimal surgical approach for a PCL reconstruction. Debate exists about the best graft type or source, placement of the tibia, femoral tunnels, number of graft bundles and the amount of tension on the bundles.[6]
Graft sources can be allograft (mostly Achilles tendon) or autologous tissue (Bone-patellar tendon-bone, quadrupled hamstring or quadriceps tendon).[6]
The most common autologous graft is the bone-patellar tendon-bone, because the bone plugs allow sufficient fixation of the tissue. The disadvantages of this graft are the harvest site morbidity and because the graft has a rectangular form, the tunnels can’t be completely filled with collagen. Using the hamstring graft decreases the morbidity factor, but results in an inferior fixation method. The quadriceps tendon graft also has morbidity and has adequate biomechanical properties.
Allografts provide a decreased surgical time and the absence of iatrogenic trauma to the harvest site. The Achilles tendon graft produces a large amount of collagen. This ensures a complete filling of the tunnels.[6]
When using a double bundle graft, the two bundles of the PCL, the anterolateral and posteromedial bundle, can be reconstructed. A single bundle graft reconstructs only the stronger anterolateral bundle. The double bundle approach can restore normal knee kinematics with a full range of motion, the single bundle restores the 0° to 60° knee flexion.[10]
The tibial inlay procedure starts with a diagnostic arthroscopy, but the inlay itself is an open surgery. The femoral tunnels are established with an outside-in technique to closely duplicate the femoral insertion of the PCL-meniscofemoral ligament complex. The graft is prepared during the exposure. Then it is placed in the graft passer and passed through the femoral tunnel, tensioned and screwed to the bone.
After the surgery, the patients have to wear a brace, locked in full extension. After four weeks, the brace is unlocked. A second brace is fitted after four to six weeks. This is a PCL functional brace. At the same time the crutches are discontinued. This approach is shown to be safe, with respect to the popliteal artery.[10][6]
The tibial tunnel method is an arthroscopically approach. A guide pin is drilled from a point just distal and medial to the tibial tubercle and aimed at the distal and lateral aspect of the PCL footprint. The femoral tunnel should be placed just under the subchondral bone, to reduce the risk of osteonecrosis. The direction of the graft passage depends on the type of graft used. The tibial inlay procedure avoids this difficult part. The graft is placed in 70° to 90° flexion. In the single bundle reconstruction only 1 tunnel is drilled. In a double-bundle reconstruction two tunnels are drilled, which is technically more challenging.[10][6]
Usually the Achilles tendon allograft is used to reconstruct the AL bundle and a double semitendinosus tendon autograft is used for the PM bundle reconstruction. The AL graft is tensioned and fixed at 90° flexion and the PM graft at 30°.[10]
The primary goal of the reconstruction is to correct the posterior tibial laxity.[6]
Possible complications after or during a PCL reconstruction are fracture, injury of the popliteal artery, deep vein thrombosis, residual laxity and smaller range of motion.[6] Residual laxity can be caused by an undiagnosed non-isolated PCL injury.
Range of motion problems can be caused by improper placement of the graft or too much tension. It can be treated with physical therapy or manipulation under anesthesia.[6]
Physiotherapy management[edit | edit source]
Non-operative management
According to the study of Rosenthal et al.[4] isolated PCL injuries of all degrees can be managed without surgical interventions[4], whereas Fanelli et al. only treat grade I or II PCL injuries in their practice without surgical intervention.[38] Goals for rehabilitation include reducing pain and inflammation, reducing knee joint effusion, restoring range of motion, early weightbearing and regaining strength, especially of the quadriceps muscle group.[4][6] Strengthening the quadriceps is a key factor in a successful recovery, because the quadriceps can take the place of the PCL to a certain extent, helping to prevent the femur from moving too far forward over the tibia.
The focus of rehabilitation can lie on the quadriceps muscle group, or on the whole lower extremity, where the hamstrings muscle group is also involved.. In both manners, the eccentric strengthening of the muscle group(s) should be included in PCL rehabilitation.[4][6]
Herefore, closed chain excercises are recommended for grade I and II PCL injuries. They do not only increase muscle strength, but also have a positive effect on balance, proprioception and coordination. Once the strength and endurance has been regained and the neuromuscular control has been increased, the patient can move on to an agility based program.[4]
Grade I and II PCL injuries have a rather rapid recovery and patients should be able to get back to sports within two to four weeks of injury. Grade III PCL injuries recover much slower and, depending on the sport, patients are usually able to return to sport after three months.[4]
Patients with a grade III PCL tear are usually immobilized in full extension for the initial two to four weeks. This eliminates posterior subluxation caused by the hamstrings, which causes the injury to remain isolated and therefore can be managed without surgical intervention.[4]
Physical therapy starts with basic quadriceps setting and straight les raises. At two to four weeks, active assistive motion can begin along with advancing to weight bearing within the pain limit. The focus in this therapy lies mainly on quadriceps based excercises to promote dynamic stabilization and hereby counteract posterior tibial subluxation. Flexion past 70° and isolated hamstring strengthening are initially avoided. The therapy evolves from closed chain excercises (CKC) to addition of eccentric open kinetic chain (OKC) excercises and eventually functional excercises such as biking, leg press, elliptical excercises and stair climbing.[4][6]
Patients that are not able to progress to this functional level of excercises and continue to have pain may need surgical intervention.[4]
Post-operative rehabilitation
Post-operative rehabilitation typically spans six to nine months. The duration of each of the five phases and the total duration of the rehabilitation depends on the age and physical level of the patient and on the success of the operation The rehabilitation starts with focussing on protecting the PCL-graft by placing the knee in a hinged ROM knee brace locked in extension during the first few post-operative weeks. The brace may only be unlocked while sitting or while performing ROM and strengthening excercises.
In the immediate post-operative phase, passive knee flexion and active knee extension are encouraged from 0° to 90°. Isometric quadriceps excercises, straight leg raises (SLR) and hamstrings stretching excercises can herefore be performed. These excercises are typically repeated three to four times a day, each series consisting of 10 to 25 repetitions.[4][6]
Knee effusion should be closely monitored, since it significantly contributes to muscle atrophy and inhibition. The primary modality to manage this effusion is the RICE-method: Rest, Ice, Compression, Elevation. The ice should be applicated 10 to 20 minutes every two to four hours, along with elevation and compression. (this is a standard procedure, but is not based on scientific evidence; Level of evidence:5) To restore ROM and prevent arthrofibrosis, patella mobilizations should be performed in all directions during the early phases of rehabilitation.[4][6]
In the next phase – the maximum protection phase – ROM should progress from 0° tot 120° and weightbearing should progress from weightbearing as tolerable (WBAT) with crutches to full weight bearing without crutches. The following criteria should be met to discontinue crutches: good quadriceps control, no extension lag during a SLR excercise, full ROM in extension, ability to do single leg stance without pain of unsteadiness and a non-antalgic gait. In this phase it is also important to normalize gait, especially the loading and stance phases with quadriceps activation. In this maximum protection phase OKC knee extension excercises (range 0° to 70°) and CKC weight bearing excercises (range 0° to 45°) are performed. These early closed kinetic chain excercises can include squatting, bilateral and unilateral leg press. Once knee flexion is greater than 100°, the patient can ride the stationary bike. Pool therapy, SLR excercises using resistance of max. 10% of the bodyweight and leg presses and mini-squats (0° to 45° knee flexion) can be incorporated as additional strengthening excercices. Leg presses and mini-squats can be progressed form double to single limb support. The rice-method should also be continued during this second phase.[4]
In phase three – the controlled ambulation phase – CKC excercises are progressed from bilateral to unilateral within a knee flexion range of 45° to 60°. Excercises such as wall squatting, single leg squats and lunges, progressed by adding resistance, increase ROM. The knee brace should be discontinued in the first half of this phase. Other excercises including balance and proprioceptive drills, forward and lateral step-ups, chair climbing, treadmill walking and pool jogging are performed during this phase. Resisted knee flexion excercises should only be performed at the end of the phase, because of the great shear force on the PCL during this movement.[4]
During the fourth phase – the light activity phase – a progression is made from walking to running and light agility drills are added to the program. These drills include line hops, bounding and ladder drills. The progression from walking to jogging can be made once following criteria are met: normal gait, knee ROM range from 0° to 120°, no joint effusion, ability to do single leg hops without pain and walking tolerance of minimum 25 minutes. During this phase, ROM, speed, resistance and/or volume or duration of the excercises should be increased. Knee and hip strengthening excercises should be continued and other excercises should be added, such as OKC quadriceps excercises (range 90° to 0°), OKC hamstring excercises (range 0° to 45°) and CKC squatting and lunging (range 0° to 75°). Swimming and agility drills in water are initiated and continued throughout this phase. Before the patient can return to sports (phase five), he/she should be able to perform a hop test with an outcome of minimum 80% compared to the unaffected limb.[4]
The last phase of rehabilitation – the return to sport phase – increases strengthening excercises and neuromuscular control demands. Examples of excercises during this phase are multi-directional lunges, single leg stance with perturbation, running, change of direction drills and bench or box jumps. Sport specific activities in this phase incorporate movements in the sagittal, frontal and transverse planes. CKC excercises advance into the range of 0° to 90° and OKC hamstring excercises are now performed in the range of 0° to 60°. High impact activities can be performed in this phase, two to four times a week. To determine whether the patient is able to return to sport, therapists prefer hop testing. The outcome of this test should be minimum 90% compared to the unaffected limb. During this test, the jumping and landing of the patient should be observed to avoid hyperextension and varus or valgus angulation.[4]
When the physical therapy sessions are over, patients should be aware of the importance of the home excercise program they should keep following.. During their sport activities, patients may use a functional knee brace to increase proprioception and facilitate normal knee mechanics during running and pivoting activities. However, the effect of such a brace has not been scientifically proven.[4]
Resources[edit | edit source]
- http://emedicine.medscape.com/article/90514-overview
- http://orthoinfo.aaos.org/topic.cfm?topic=a00420
- http://emedicine.medscape.com/article/1252128-overview#a0112
- http://www.sportsmd.com/Articles/tabid/1010/id/10/Default.aspx?n=pcl_tear_( posterior_cruciate_ligament)#sthash.k6uCPX0x.N6yQajOD.dpbs
- http://www.sportsinjurybulletin.com/archive/pcl-injuries#
- http://msdlatinamerica.com/ebooks/ChapmansOrthopaedicSurgery/sid1101681.html
Clinical Practice Guidelines: Knee Ligament Sprain Revision 2017
- Chandrasekaran S, Ma D, Scarvell JM, Woods KR, Smith PN. A review of the anatomical, biomechanical and kinematic findings of posterior cruciate ligament injury with respect to non-operative management. The Knee. 2012 Dec;19(6):738-745.
- Harner CD, Höher J. Evaluation and treatment of Posterior Cruciate Ligament Injuries. The American Journal Of Sports Medicine. 1998 May; 26(3): 471-482.
- Malone AA, Dowd GSE, Saifuddin A. Injuries of the posterior cruciate ligament and posterolateral corner of the knee. Injury, Int. J. Care Injured. 2006, 37: 485-501.
- Lubowitz JH, Bernardini BJ, Reid JB. Current concepts review: comprehensive physical examination for instability of the knee. The American Journal of Sports Medicine. 2008 Mar;36(3):577-594.
- Wind WM, Bergfeld JA, Parker RD. Evaluation and Treatment of Posterior Cruciate Ligament Injuries Revisited. The American Journal of Sports Medicine. 2004, 32(7): 1765-1775.
Clinical bottom line[edit | edit source]
PCL injuries do not occur frequently. The reasons for this are the strenght of the ligament and the fact that hyperflexion, possible through a force to the anterior aspect of the proximal tibia, does not commonly occur. Hyperflexion is, however, one of the possible causes for a PCL injury. Therefore such an injury will mostly happen during sports, such as football, soccer and skiing. Another cause can be a car accident, resulting in a 'dashboard injury'. The severity is divided in three degrees and an acute injury is distinguished from a chronic injury. Clinical presentation will depend on the degree and the condition of the injury. If symptoms are observable, these usually include swelling, pain, feeling of instability, limited range of motion and difficulty in walking. The treatment depends on the grade and the individual patient. A grade I and II injury are usually treated non-surgically. A grade III injury is usually treated by a surgical intervention, however non-surgical treatment is also possible. Physical therapy depends on whether there has been an operation or not. Both rehabilitation programs focus on the quadriceps muscle group, because of its ability to partially take over the function of the PCL. The structure and the build-up of the rehabilitation program depends on the degree of the injury, the individual patient and the succes of the operation in case this was necessary.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 Medscape. Drugs & Diseases, Sport Medicine. Posterior Cruciate Ligament Injury. https://emedicine.medscape.com/article/90514-overview (accessed 20/08/2018).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Paulsen F, Waschke J, Sobotta. Lower extremities, Knee Joint. Elsevier, 2010. p 272-276.
- ↑ 3.0 3.1 Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Archives of orthopaedic and trauma surgery 2003;123(4):186-91.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 Lee BK, Nam SW. Rupture of Posterior Cruciate Ligament: Diagnosis and Treatment Principles. Knee Surgery and Related Research 2011 Sep;23(3):135-141.
- ↑ 5.0 5.1 5.2 American Academy of Orthopaedic Surgeons. Diseases & Conditions: Posterior Cruciate Ligament Injuries. http://orthoi/nfo.aaos.org/topic.cfm?topic=a00420 (accessed 20/08/2018).
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 6.19 6.20 6.21 Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. The American Journal of Sports Medicine 1987;15(6):553–557.
- ↑ 7.0 7.1 7.2 Malone AA, Dowd GSE, Saifuddin A. Injuries of the posterior cruciate ligament and posterolateral corner of the knee. Injury 2006;37(6):485-501.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Bisson LJ, Clancy Jr WG. Chapter 90: Isolated posterior cruciate ligament injury and posterolateral laxity. In: Chapman’s Orthopaedic Surgery. 3rd edition. Philadelphia: Lippincott Williams & Wilkins 2001.
- ↑ 9.0 9.1 British Medical Journal Best Practice. Evaluation of knee injury. https://bestpractice.bmj.com/topics/en-us/575 (accessed: 22/08/2018).
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 Wind WM, Jr, Bergfeld JA, Parker RD. Evaluation and treatment of posterior cruciate ligament injuries: revisited. The American Journal of Sports Medecine 2004, 32(7):1765–1775.
- ↑ Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.
- ↑ Physiotutors. Posterior Sag Sign | Posterior Cruciate Ligament Tear. Available from: https://www.youtube.com/watch?v=7vgTMnfP4fs
- ↑ Physiotutors. Posterior Drawer Test⎟Posterior Cruciate Ligament. Available from: https://www.youtube.com/watch?v=wDIGll5wzZs